lisaray
Guest
I bill for MD AND APRN'S who are behavioral health providers. so Psychiatrist and Psych NP's. Anyway one particular MA plan in which we bill E and M codes for follow up medication management started charging copays when their services dates had no copay before earlier in the 2024 Calendar Year. CPT, Place of service everything is the same. So I questioned the Medicare Advantage plan as to why this had changed three to four months into the year. It took them months to answer. 1st response was as follows:
This was reviewed by our Benefits team. There are two pieces to this:
The inconsistency is due to an update to Benefits that did take place around March. The cost share patients are now receiving is correct.
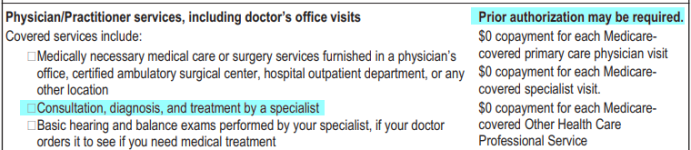
If your providers bill an E&M code (99212-99215), that will take a Specialist co-pay, as the visit is considered a Specialty visit. If the provider bills a psych code (90834, 90837, 90791, 90792) they will not receive a co-pay, as it is considered a Behavioral Health visit.
So then I asked.them f they notified their members or providers in writing of this benefits change and when was the exact date that this change took place. No answer again for weeks. I keep pushing and this is what they sent me.
Hello Lisa,
I have verified that Rachaels guidance previously provided is accurate as to how Cigna Medicare is applying benefits to E&M codes. They have made the change to follow CMS guidelines on 4/3/24. When providers bill an E&M code (99212-99215) for Cigna Medicare members, that will take a Specialist co-pay, as the visit is considered a Specialty visit. If a provider bills a psych code (90834, 90837, 90791, 90792) they will not receive a co-pay, as it is considered a Behavioral Health visit according to CMS guidelines. Cigna Medicare did not send notifications to members or providers as they are following CMS guidelines. If they have any additional questions or concerns regarding this change please contact Cigna Medicare directly
Problem is I called and chatted with Medicare and they can't find any guideline changes that were issued in April of 2024. it is no where to be found. Here is where it gets interesting. they have changed their members cost shares. according to MA plan guidelines
No, Medicare Advantage (MA) organizations are not allowed to make midyear changes to non-prescription drug benefits, premiums, and cost-sharing.
In addition Medicare does not mandate or oversee guidelines for copays with medicare advantage plans.
So I don't think that what this MA PLAN has been telling me is correct and if they are not supposed to make changes midway through the year to members benefits it seems what they are doing is contrary to CMS policy. For example Medicare does not change the deductible amount part of the way through the year
Does anyone know who I should reach out to ? Medicare is unable to find this CMS guideline change that the MA plan bases or uses as the rationale for charging the copay or cost share to patients that they never had before.
Seems fishy to me.
This was reviewed by our Benefits team. There are two pieces to this:
The inconsistency is due to an update to Benefits that did take place around March. The cost share patients are now receiving is correct.
If your providers bill an E&M code (99212-99215), that will take a Specialist co-pay, as the visit is considered a Specialty visit. If the provider bills a psych code (90834, 90837, 90791, 90792) they will not receive a co-pay, as it is considered a Behavioral Health visit.
So then I asked.them f they notified their members or providers in writing of this benefits change and when was the exact date that this change took place. No answer again for weeks. I keep pushing and this is what they sent me.
Hello Lisa,
I have verified that Rachaels guidance previously provided is accurate as to how Cigna Medicare is applying benefits to E&M codes. They have made the change to follow CMS guidelines on 4/3/24. When providers bill an E&M code (99212-99215) for Cigna Medicare members, that will take a Specialist co-pay, as the visit is considered a Specialty visit. If a provider bills a psych code (90834, 90837, 90791, 90792) they will not receive a co-pay, as it is considered a Behavioral Health visit according to CMS guidelines. Cigna Medicare did not send notifications to members or providers as they are following CMS guidelines. If they have any additional questions or concerns regarding this change please contact Cigna Medicare directly
Problem is I called and chatted with Medicare and they can't find any guideline changes that were issued in April of 2024. it is no where to be found. Here is where it gets interesting. they have changed their members cost shares. according to MA plan guidelines
No, Medicare Advantage (MA) organizations are not allowed to make midyear changes to non-prescription drug benefits, premiums, and cost-sharing.
In addition Medicare does not mandate or oversee guidelines for copays with medicare advantage plans.
So I don't think that what this MA PLAN has been telling me is correct and if they are not supposed to make changes midway through the year to members benefits it seems what they are doing is contrary to CMS policy. For example Medicare does not change the deductible amount part of the way through the year
Does anyone know who I should reach out to ? Medicare is unable to find this CMS guideline change that the MA plan bases or uses as the rationale for charging the copay or cost share to patients that they never had before.
Seems fishy to me.