According to my encoder software all 3 of the procedure codes, 0660T, 66174 & 66984, are subject to MPR with a payment indicator of 2.

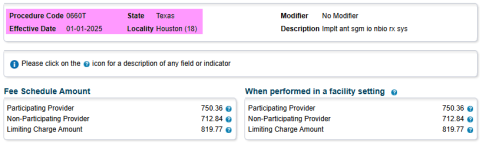
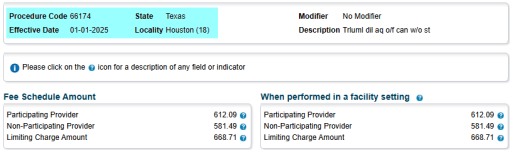
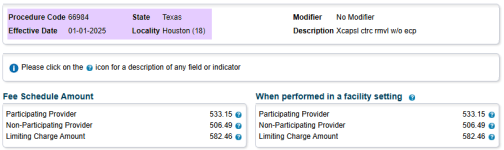
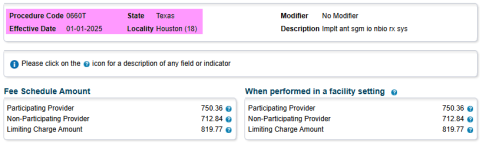
You are correct there aren't any RVUs for 0660T since it is a new category III code, but the payment indicator of 2 indicates you should rank each procedure by fee schedule amount. Additionally, the pricing indicator for 0660T is based on carrier pricing for Medicare Part B. So the question I have for you is, what are your fee schedule allowances for your MAC for each of these 3 CPT codes. Once you list the procedures in order based on the fee schedule allowances and then from there bill your highest fee schedule procedure as the primary procedure and then the remaining 2 procedures should be billed with modifier 51 for MPR.
I'm guessing the 0660T is potentially the procedure with the highest fee schedule allowance since you are being reimbursed at 100% of what I assume is the billed charge based on the fact that you didn't indicate any type of reduction between the billed charge and the amount being paid by the carrier. If this is the case you would bill 0660T as primary and then add modifier 51 to the remaining 2 procedures so that 50% MPR is applied to these codes, as they likely have a lower fee schedule allowance.
Is 0660T your highest cost procedure of the 3 codes you've listed? If so, then it makes sense that you are not seeing reductions for 0660T when billed in conjunction with 66174 & 66984.
Based on your profile location of Houston, TX, it appears your Part B MAC is
Novitas Solutions carrier code 04412, locality 18., I've linked their web page for their carrier/contractor priced procedures fee schedule. This list only applies to procedures which have been designated by Medicare as being based on the local carrier/contractor pricing fee schedule. You can either download the fee schedule from the link above or you can use the fee schedule calculator, which does include the pricing for 0660T. Here is a link to the calculator.
Medicare JH Jurisdiction.
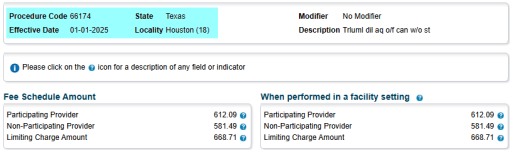
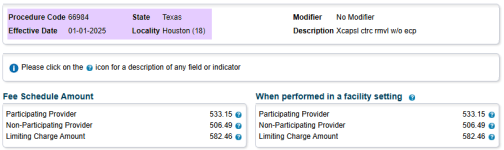
Here is the fee schedule allowances for each of your CPT codes:
I hope this information is helpful to you and your practice.