ejhahn
Contributor
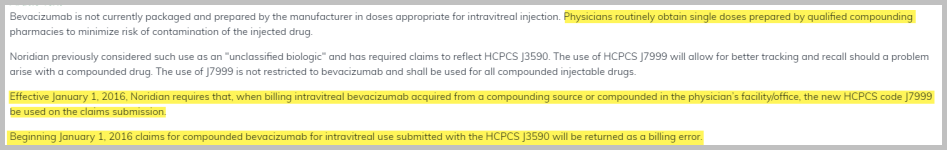
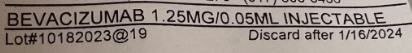
Hi - We bill for an ophthalmologist's office and are needing help with how to bill a compound drug. This drug is used like Avastin, but we receive from a compound pharmacy, so do not have an NDC #. We receive a single-dose vial that is 1.25MG/0.5ML, so cannot bill code J3590. Medicare has guidance stating we can code HCPCS J9035, but other insurances have denied. Because it's a compound drug, would we bill J7999 for any insurance that does not follow CMS guidelines? Any input would be appreciated!
Thank you!
Thank you!