tfypoo
New
A patient was seen to have 2 Nexplanon devices removed. Can you bill the removal procedure twice?
Please provide a description of the procedure performed (ie, providers notes) so we can better help you with this.A patient was seen to have 2 Nexplanon devices removed. Can you bill the removal procedure twice?
HPI - The patient presents today for Nexplanon removal. She has two devices in place in her left arm. She was previously counseled, and all questions have been answered to her satisfaction.Please provide a description of the procedure performed (ie, providers notes) so we can better help you with this.
Yes that is the code we use for a Nexplanon removal. My question is since the patient has 2 Nexplanon implants in her arm can I bill 11982 twice.Have you looked at 11982?
Thank you!There is a MUE on 11982 of 1. Based on the documentation, there was 1 incision made. I don't even see enough there to try to justify -22 on the removal. I would bill this 11982 only once.
I would report 11983 with a modifier -22 if the removal time was significant. If is was just slipped in and immediately slipped out I think I would report 11983 with no modifier. If you are being reimbursed by the manufacturer you should not be billing insurance. But you could bill insurance, and if they refuse to pay, contact the manufacturer.does anyone know how to charge for a removal and insertion and removal again in the same visit because she had numbness from hitting a nerve when they reinserted the new one so immediately removed the new one.
also I was told you could get reimbursement from the manufacturer for the Nexplanon and told to charge the device to insurance. but i would think if we're getting reimbursed from the manufacturer not to charge insurance because wouldn't that be double dipping?
Thank you a ton as always!I would report 11983 with a modifier -22 if the removal time was significant. If is was just slipped in and immediately slipped out I think I would report 11983 with no modifier. If you are being reimbursed by the manufacturer you should not be billing insurance. But you could bill insurance, and if they refuse to pay, contact the manufacturer.
No one is asking about charging and E/M code. So I'm curious. My providers are charging a 99212. Does anyone else charge e/m codes with insertion, removal or both?I would report 11983 with a modifier -22 if the removal time was significant. If is was just slipped in and immediately slipped out I think I would report 11983 with no modifier. If you are being reimbursed by the manufacturer you should not be billing insurance. But you could bill insurance, and if they refuse to pay, contact the manufacturer.
I would charge an E&M only if an E&M was provided. At whatever level was documented. Always a 99212 (or any "always" level) makes me raise an eyebrow.No one is asking about charging and E/M code. So I'm curious. My providers are charging a 99212. Does anyone else charge e/m codes with insertion, removal or both?
Unless there's a separate issue addressed and enough e/m for it then I don't charge an e/m. There's a small amount of e/m already built into procedures already, so if they are there for just that and it's just the procedure I just charge the procedure. Also often times counseling done regarding the procedure was done prior to the visit for my practice.No one is asking about charging and E/M code. So I'm curious. My providers are charging a 99212. Does anyone else charge e/m codes with insertion, removal or both?
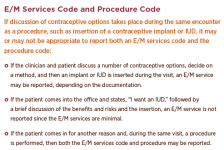
ACOG has a LARC coding guideline, but to reiterate what was said above, a provider should not be standardly charging an E+M in this situation. Here is a snip from a PDF versionNo one is asking about charging and E/M code. So I'm curious. My providers are charging a 99212. Does anyone else charge e/m codes with insertion, removal or both?
Thank you!I would charge an E&M only if an E&M was provided. At whatever level was documented. Always a 99212 (or any "always" level) makes me raise an eyebrow.
From the original poster here, the documentation supplied was a procedure only and would not support any E&M level.
Thank you!ACOG has a LARC coding guideline, but to reiterate what was said above, a provider should not be standardly charging an E+M in this situation. Here is a snip from a PDF version
View attachment 7059
Thank you!Unless there's a separate issue addressed and enough e/m for it then I don't charge an e/m. There's a small amount of e/m already built into procedures already, so if they are there for just that and it's just the procedure I just charge the procedure. Also often times counseling done regarding the procedure was done prior to the visit for my practice.