Hey Brandi,
It has been a while since I have done E&M chart reviews for FP/Internal Med. and, I am needing help understanding the examination portion of the review. Can you help me understand:
-When it says at least 2 bullets of 9 systems does that mean the doctor has to write something?
-Does that differ from when the doctor check marks all the WLN on all the systems without writing anything beside the system?
-Or if he checks all but 2 WLN and rights by that system a description like Lung sounds clear does that count as a bullet?
The other section that I need clarification is the number of diagnosis section. I give a point for every dx?
ex: htn - chronic stable 1 point
dmII- chronic stable 1 point
copd - chronic worsening 2 points
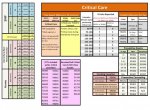
I pulled up the audit sheet you use and it says only count how many dx billed to determine points. Not by if it is new problem, est problem etc.
I have read trailblazer guidelines but, it doesn't break it down enough to where I can understand it. You seem to know your stuff and could really use your help!!!!!!!!
If it is easier to walk me through via phone I would gladly take your expertise!!
Thank you!!!
-When it says at least 2 bullets of 9 systems does that mean the doctor has to write something?
-Does that differ from when the doctor check marks all the WLN on all the systems without writing anything beside the system?
-Or if he checks all but 2 WLN and rights by that system a description like Lung sounds clear does that count as a bullet?
What you're describing is crappy documentation, from over-utilizing a template. No, he doesn't technically have to write anything, if there's nothing to write - except in the system pertaining to the chief complaint. [WLN is considered a 'pertinent negative' finding when it's related to the system that's supposed justify the reason for the visit. Documentation of WLN without further explanation there is considered insufficient.]
If the plan, HPI, or ROS indicate that there was a problem, he's taking a risk by not documenting his relevant exam findings. I wouldn't count it as valid in that case. (Also, he'd probably benefit more from utilizing the 95 guidelines, from that sound of things)
"Lungs clear" gets a bullet for Auscultation of Lungs
The other section that I need clarification is the number of diagnosis section. I give a point for every dx?
ex: htn - chronic stable 1 point
dmII- chronic stable 1 point
copd - chronic worsening 2 points
I pulled up the audit sheet you use and it says only count how many dx billed to determine points. Not by if it is new problem, est problem etc.
Look to the HPI - these are chronic conditions, so he should have documented which conditions were being managed in the follow-up visit, their treatment plans, and status, as well as any symptomatic episodes since the last visit. (If he didn't, then don't count them in the number of chronic conditions for HPI. I'd advise him of the correct way to document chronic condition HPI for future reference, since HPI elements are really more for utilization with new conditions, and acute episodes, to paint the full picture needed, to ascertain the characteristics of the problem, that led him to take the actions he took, to determine a diagnosis)
If he didn't address a condition in the HPI, don't count it for MDM. Just because a patient has a condition, doesn't mean he made a decision on it. It might complicate the decision he needs to make regarding another condition (for example, if he were removing a corn for a diabetic patient, the diabetes would be a risk factor, since it complicates the healing, but he wouldn't get separate credit for it under the # of Dx section, simply because it exists). If there's not a clear link between what he did to manage the condition from the chief complaint, and a risk posed by the other conditions listed, don't count them at all. They're just informative, in that case.
If he at least mentioned all 3 in the HPI, and documented their status and current treatment plans somewhere in the note, all of that gets 3 point under the first box.