Queizati
Networker
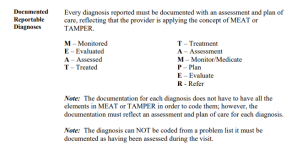
Hi all, we have a physician who documents in a way that is causing me to second-guess what is the most appropriate and accurate diagnosis code to assign for each visit. The note contains an assessment and plan where the physician free texts the patient's condition, however, the physician then utilizes a function in the EMR that pulls into the note the ICD-10 descriptor(s) for every ICD-10 code selected for the encounter by the physician. Essentially, all associated diagnoses that appear in charge entry have been transferred into the note (along with all associated orders).
As a coder, where do we abstract from? Initially, I was coding the sign/symptom/condition as stated by the physician in their narrative under the A&P. Now, I am having second thoughts on whether we can use the diagnosis codes in the 'Problem List Items Addressed This Visit'. As you can see in examples #2 and #3, the physician is using verbiage that indicates uncertainty per ICD guidelines, which would be coded to the sign or symptom, yet there are diagnoses on this problem list for the visit.
Any feedback or insight would be much appreciated.
As a coder, where do we abstract from? Initially, I was coding the sign/symptom/condition as stated by the physician in their narrative under the A&P. Now, I am having second thoughts on whether we can use the diagnosis codes in the 'Problem List Items Addressed This Visit'. As you can see in examples #2 and #3, the physician is using verbiage that indicates uncertainty per ICD guidelines, which would be coded to the sign or symptom, yet there are diagnoses on this problem list for the visit.
Any feedback or insight would be much appreciated.
diagnosis codes, diagnosis coding