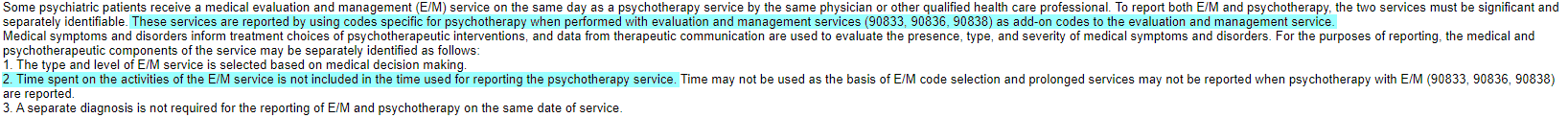
90833 is in the CPT code range for individual psychotherapy services and it is an add-on code for E&M services rendered to the patient on the same day with the same practitioner. Here is a snip of the CPT section guidelines regarding code range 90832-90838.
View attachment 6676
View attachment 6677
So, to answer your question, no you shouldn't have to specifically state that the session is individual vs. group since the code is specifically for individual psychotherapy services and the clinical documentation should support that the services were for individual psychotherapy.
Also, you need to make sure the documentation for the time spent on the individual psychotherapy is separate from the time the provider spent on the E&M service that is the primary code for billing 90833. If the patient did not receive E&M services on the same day from the same practitioner, then you need to look at 90832, which represents the same amount of time for the individual psychotherapy visit but it is a stand-alone code. Your posting indicates what the current documentation is for your use of 90833 but nothing indicates that the E&M service happened that is required to bill 90833.
I don't know if this was intentionally left out of your post, or if the E&M services are not being rendered to the patient by the same practitioner on the same DOS as the 90833 but if the patient is not receiving the E&M services you need to revisit your code selection for the individual psychotherapy services. If you are receiving reimbursement currently for billing 90833 without the E&M, eventually the insurance companies are going to realize there is an issue and you'll more than likely start receiving denials for billing an add-on code without the appropriate primary code and you may receive overpayment requests for the claims that were previously paid in error.