Can anyone help me with why my nurse injection codes are being rejected by Medicare? The reason given on the EOB is missing referring provider name/identifier. I'm billing for internist so there is no referring physician. Contacted Medicare and they are reviewing but in the meantime my rejections are adding up.
-
If this is your first visit, be sure to check out the FAQ & read the forum rules. To view all forums, post or create a new thread, you must be an AAPC Member. If you are a member and have already registered for member area and forum access, you can log in by clicking here. If you've forgotten your username or password use our password reminder tool. To start viewing messages, select the forum that you want to visit from the selection below..
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Wiki 96372
- Thread starter sus008
- Start date
snjberry
Networker
Some times the internist can be the referring. I have some things I bill for with my surgeon like labs in office that require a referring md...I always put him as the referring. They will deny if he cant self refer however, some codes can have self referral
Hope this helps. You could try one and see if it pays.
Sandi
Hope this helps. You could try one and see if it pays.
Sandi
btadlock1
Guest
Can anyone help me with why my nurse injection codes are being rejected by Medicare? The reason given on the EOB is missing referring provider name/identifier. I'm billing for internist so there is no referring physician. Contacted Medicare and they are reviewing but in the meantime my rejections are adding up.
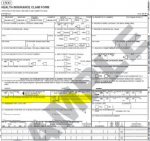
Check out the picture I attached - (Sorry about the crooked highlighter - drawing a straight line on a laptop touchpad is harder than you might think) -Since there was no referring provider, and you obviously can't leave it blank, try putting "N/A" in box 17 (name) - if it still won't go, then put your own doctor's info in 17, 17a, and 17b. Self referral isn't allowed for ancillary services that fall under Stark Laws, but other services are okay.
If your claims are electronic -which they should be - then you need to tell your electronic claims/IT person to check the transaction code sets,
Tell them to check Loop 2310A, to see if it's going through on the claim. Take it out if it is.(It's complicated to figure out, so I'm not going to explain it all here, but if you need help finding information on it, let me know.)
http://www.dmap.state.de.us/downloads/forms/ECS Guidelines.pdf
I don't know if Medicare requires it on every claim, but that's something you should check. I'll look around and see if I can find the rule on this issue and get back to you.
Attachments
btadlock1
Guest
Found it! It's not required...
There it is!
http://www.cms.gov/transmittals/downloads/R1251CP.pdf
"Carriers and MACs shall accept paper (from those providers still permitted to submit paper claims under ASCA), and electronic claims for ambulance services submitted without the name or an NPI for a referring or ordering physician in the fields, segments and loops as described above."
This kind of shows what the field looks like - I suggest that everyone who can find the time learn how the X12 transaction code sets work; it's valuable information.
http://www.eedi.net/837004010X097A1/172_837004010X097A1.htm
There it is!
http://www.cms.gov/transmittals/downloads/R1251CP.pdf
"Carriers and MACs shall accept paper (from those providers still permitted to submit paper claims under ASCA), and electronic claims for ambulance services submitted without the name or an NPI for a referring or ordering physician in the fields, segments and loops as described above."
This kind of shows what the field looks like - I suggest that everyone who can find the time learn how the X12 transaction code sets work; it's valuable information.
http://www.eedi.net/837004010X097A1/172_837004010X097A1.htm
All ancillary services for Medicare require a "referring physician". I bill for a family practice physician and I use her for the referring as she requested the additional testing is to be done. Urinalysis, EKG's etc. need to have them added to the claim for Medicare only.
Pam Porter, CPC
Pam Porter, CPC