Hello
sdaniels,
Again, I will try to assist you. From the final interpretation without seeing the gross or microscopic I cannot clearly tell the difference between 88305 or 88307. I'd like to pretend it is a punch skin biopsy, but I really do not know reviewing the information provided. The gross and microscopic (with no PHI would assist). The reason(s) why I state this is because ~ let's review specimen A & B together with this information.
Were these skin biopsies, or breast lesions with margins reviewed?
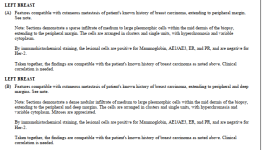
A) states within the final interpretation that "patient's history of breast carcinoma, extending to peripheral margin"
B) states within the final interpretation that "patient's history of breast carcinoma, extending to peripheral & deep margins"
Next let's discuss the immunohistochemical stains:
Specimen A:
Mammoglobin, AE1/AE3, ER, PR, HER2 were either positive or negative (no quantification provided)
Specimen B:
Mammoglobin, AE1/AE3, ER, PR, HER2 were either positive or negative (no quantification provided)
Coding stains can be horribly cumbersome sometimes, so I'll walk you through this.
Specimen A: You bill 88342x1 for the Mammogloblin, 88341x4 (for the AE1/AE3, ER, PR, HER2)
Specimen B: You bill 88342x1 for the Mammogloblin, 88341x4 (for the AE1/AE3, ER, PR, HER2)
Let me summarize:
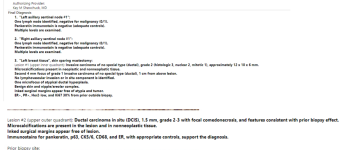
If this was a skin for example punch biopsy from two different sites we would bill at the end of the day
88305x2
88342x2
88341x8
If this was deemed a breast lesion with margins reviewed (not shared so unsure here???)
88307x2
88342x2
88341x8
Again, let me reiterate what I know. If the immunohistochemical stain is postive or negative (it is a qualitative stain). The first charge is billed with 88342 with subsequent charges billed with 88341.
If someone felt that 88360 (from your example above) was warranted to be billed it CLEARLY should have been displayed within the pathology report in a quantitative state (%, numerical, or otherwise here).
There is absolutely no way to support 88360 with a positive or negative finding unless you have THAT NECESSARY QUANTIFICATION. (If it was the pathologist's questioning ~do not be shy, many are so incredibly kind, just explain that you need a quantitative state to capture RVU's for getting CPT 88360 if you possibly felt they missed that opportunity.
Most do not know. Our pathologist's work super hard, and long. If I recall correctly from one of my pathologist mentors during their 8 years of training, they get that one "class in school". It clearly in my logistics isn't enough. It is a constant open communication line here from me. Since 2012 to now I still appreciate the opportunity to discuss new pathology trends
I am going to give a shout out to all those billers that appeal these scenarios. This is again the stuff that keeps me up at night and absolutely applaud every single one of you!!
The CCI edits are flooding appeals FOR ALL PAYORS because 88342, 88341 doesn't play well with 88360. Some billers have been there for so long and have taken the authority to "just" write stuff off if it is small enough and no one cares. I had so many denials that 88342 was denied because of 88360 so they wrote off the 88342 (small dollar amount I am guessing??) and now I had to deal with the other copious amounts of 88341 charges that were denied. I can provide fictious examples of this of course.
I apologize for being lengthy,
Please reach out to me if you have any questions.
Or PM me, if necessary, okay
Dana