ahodge90
Networker
I have an issue that is being debated in our clinic, and am curious what other coders have to say about this.
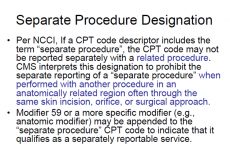
we have a case where a provider did a diagnostic scope first and then did a lateral release. we ran the NCCI edits and they are not coming up as bundled, but there is that parenthetical with 29870 that says separate procedure. My impression of this parenthetical is that if this is done on the same anatomical area they cannot be billed separately. BUT there is something that I found from what looks like an older appc presentation that makes me wonder if they can be billed together.
Can anyone help me understand this so that I can help my clinic better understand this? Can we bill the diagnostic code with an open procedure, when it was NOT converted to open?
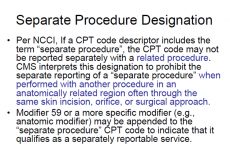
we have a case where a provider did a diagnostic scope first and then did a lateral release. we ran the NCCI edits and they are not coming up as bundled, but there is that parenthetical with 29870 that says separate procedure. My impression of this parenthetical is that if this is done on the same anatomical area they cannot be billed separately. BUT there is something that I found from what looks like an older appc presentation that makes me wonder if they can be billed together.
Can anyone help me understand this so that I can help my clinic better understand this? Can we bill the diagnostic code with an open procedure, when it was NOT converted to open?