10mcdowj
Guest
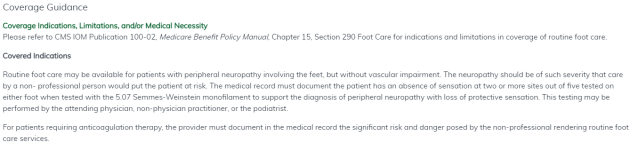
Our podiatrist is constantly wanting to bill 11055-11057 for the debridement of keratomas/hyperkeratotic tissue for diabetic patients or patients with peripheral vascular disease. From reading the guidelines, it sounds like this cpt should be covered as long as the patient has an underlying condition, which they do.
In 2019 and prior we would bill this cpt with L84 as one of the diagnoses. The LCD for 2020 updated (Medicare J5, article #A56232 on CMS) and no longer lists any related codes to L84 and doesn't give any direction on what they want instead. Some insurances have started outright rejecting this cpt if we have diagnosis L84 listed anywhere on the claim. I don't feel E11621 (or any PVD codes with ulceration mentioned) fits, as my doctor specifically mentions that there is no ulceration present, just keratomas or hyperkeratotic tissue. I also wouldn't know what to do for PVD as he often lists this diagnosis as unspecified (I739) and doesn't give any descriptions in the notes to determine a more specific code. Maybe that is another issue in itself.
Additionally, sometimes we can get this code to pay if we bill it with something in diagnosis pointer 3 such as hammertoes, pain, etc. However these codes aren't always given or supported by the notes. It also doesn't quite make sense as the hammertoe diagnoses aren't listed in the LCD either.
Ex. 11055-Q8 E1151 L84 M2041 M2042
I have done so much google/AAPC site searching, have read forum after forum, have asked several of my colleagues, reached out to other coders I know, and I'm at a loss at what to do at this point. Appeals are useless when it's an LCD denial. If it weren't getting paid some of the time, I would let our doctor know this isn't covered and advise him to start getting ABNs.
Is anyone else having this problem? If you have any inkling on what to do, please help!
In 2019 and prior we would bill this cpt with L84 as one of the diagnoses. The LCD for 2020 updated (Medicare J5, article #A56232 on CMS) and no longer lists any related codes to L84 and doesn't give any direction on what they want instead. Some insurances have started outright rejecting this cpt if we have diagnosis L84 listed anywhere on the claim. I don't feel E11621 (or any PVD codes with ulceration mentioned) fits, as my doctor specifically mentions that there is no ulceration present, just keratomas or hyperkeratotic tissue. I also wouldn't know what to do for PVD as he often lists this diagnosis as unspecified (I739) and doesn't give any descriptions in the notes to determine a more specific code. Maybe that is another issue in itself.
Additionally, sometimes we can get this code to pay if we bill it with something in diagnosis pointer 3 such as hammertoes, pain, etc. However these codes aren't always given or supported by the notes. It also doesn't quite make sense as the hammertoe diagnoses aren't listed in the LCD either.
Ex. 11055-Q8 E1151 L84 M2041 M2042
I have done so much google/AAPC site searching, have read forum after forum, have asked several of my colleagues, reached out to other coders I know, and I'm at a loss at what to do at this point. Appeals are useless when it's an LCD denial. If it weren't getting paid some of the time, I would let our doctor know this isn't covered and advise him to start getting ABNs.
Is anyone else having this problem? If you have any inkling on what to do, please help!