Radiology Coding Alert
Test Your Ear, Nose, and Throat Dx Coding With 3 Examples
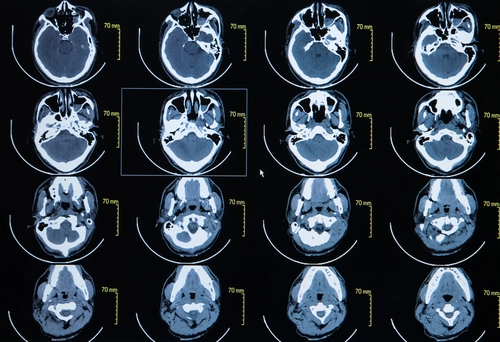
Channel your inner problem solver to simplify the coding process. Radiology coders don’t typically have a preference about coding one particular anatomic site versus another. However, the lack of frequency of maxillofacial computed tomography (CT) scans can result in some diagnoses that require pause before reaching the correct code. Coding challenge: In these instances, you’ve got to use all the tools at your disposal to code conditions of the ear, nose, and throat appropriately. Walk yourself through these three examples for a little more clarity on a few lesser reported — and often misunderstood — diagnoses. Discern Between Unspecified, Other Types of Allergic Rhinitis Diagnosis 1: The radiologist performs a CT scan for a patient with a diagnosis allergic rhinitis with fungal debris. Correctly coding this diagnosis will require you to test your problem-solving skills in addition to your understanding of rhinitis as a condition. In evaluating this diagnosis, you first want to understand that the fungal debris is not a separate diagnosis from the rhinitis, but rather a product of the rhinitis. However, this doesn’t mean that you should not consider it when making your final coding considerations. That’s because the fungal debris reveals that this is a form of allergic fungal rhinitis, and you should code it accordingly. So, instead of reporting J30.9 (Allergic rhinitis, unspecified) and disregarding the fungal debris as a symptom of the allergic rhinitis, you should be reporting J30.89 (Other allergic rhinitis) for a lack of a more specific code for allergic fungal rhinitis. “There is no code specific to allergic fungal rhinitis, which is not a fungal infection, but an allergic reaction, and reported with J30.89,” says Sheri Poe Bernard, CPC, of Poe Bernard Consulting in Salt Lake City, Utah. “When documentation simply lists ‘fungal debris’ in a patient with allergic fungal sinusitis, it should be considered an incidental finding, and no additional code is needed,” Bernard explains. “Once the fungal debris has been evaluated by pathology, you will report the appropriate ‘B’ code for the fungus that is present,” says Barbara J. Cobuzzi, MBA, CPC, COC, CPC-P, CPC-I, CENTC, CPCO, AAPC Fellow, of CRN Healthcare in Tinton Falls, New Jersey. Consider More Guidelines for Post-Tonsillectomy Bleeding Diagnoses Diagnosis 2: A patient presents to the emergency room (ER) for post-tonsillectomy bleeding. The maxillofacial CT scan reveals no further findings. As long as you know to report this diagnosis as a postsurgical complication, then you should be in the clear. There are numerous ways to find the correct code using the ICD-10-CM index. The most practical is to search the index for Hemorrhage, hemorrhagic (concealed) ⇒ postoperative, which leads you to “see Complications, postprocedural, hemorrhage, by site.” There, you’ll find hemorrhage (of) ⇒ respiratory system ⇒ following procedure on respiratory system organ or structure ⇒ J95.830 (Postprocedural hemorrhage of a respiratory system organ or structure following a respiratory system procedure). However, as long as you’re fluent with the ICD-10-CM guidelines, you know that there’s at least one more step in the coding process. When possible, you want to add specificity to the claim by reporting the patient’s actual condition as a secondary diagnosis code. Have a look at this guideline in Section C, Chapter 19 of the ICD-10-CM guidelines: Since the ICD-10-CM does not include a more specific diagnosis code for hemorrhage, or bleeding, of the tonsils, then you should not consider this guideline applicable. You should not separately report a nonspecific diagnosis code such as J35.8 (Other chronic diseases of tonsils and adenoids) in its stead. Your last consideration has to do with the aftercare code. Since the patient is still in the healing and recovery phase of the surgery, this encounter qualifies as an aftercare visit, not a follow-up visit. Therefore, you will report Z48.813 (Encounter for surgical aftercare following surgery on the respiratory system) as a secondary diagnosis. Coder’s note: ICD-10-CM explains that aftercare codes are “generally” first-listed, but this is not a requirement. In the instance that a complication diagnosis is reported in addition to an aftercare visit code, sequence the complication code first, followed by the aftercare visit code. Code Parapharyngeal Mass Depending on Pathology Results Diagnosis 3: A patient presents for a CT scan for swelling in her neck. In the impression, the physician documents a mass in the parapharyngeal space. For the sake of diagnosis coding purposes, the only information you currently have available to code is a parapharyngeal mass. In a future encounter, the patient may have a biopsy performed (with or without excision), which would allow you to report the mass as either benign or malignant depending on the pathology results. In this example, you will report J39.9 (Disease of upper respiratory tract, unspecified). Since a “mass” is nonspecific, by nature, you should not consider J39.8 (Other specified diseases of upper respiratory tract). “Industry standards and current ICD-10 guidelines indicate code assignment should be based upon the definitive pathology diagnoses,” explains Ronda Tews, CPC, CHC, CCS-P, AAPC Fellow, director of billing and coding compliance at Modernizing Medicine in Boca Raton, Florida. “The Official Guidelines for Reporting ICD-10-CM indicates that codes titled ‘other’ or ‘unspecified’ should only be used when the information in the medical record is insufficient to assign a more specific diagnosis code or a more specific code does not exist,” relays Tews.
Related Articles
Radiology Coding Alert
- ICD-10-CM Updates:
Refresh Your ICD-10-CM Coding Inventory With Brand-New Updates
See the huge variety of new codes that’s in store for you. On the surface, [...] - Guidelines:
Stay Compliant By Staying Up-To-Date on New TC, PC Billing Policy
See how these guidelines will impact your day-to-day operations. Sometimes, policy changes within the coding [...] - Case Studies:
Test Your Ear, Nose, and Throat Dx Coding With 3 Examples
Channel your inner problem solver to simplify the coding process. Radiology coders don’t typically have [...] - You Be the Coder:
Don't Stray Far From Dictation Report Diagnoses
Question: If you’ve got a report without a diagnosis that meets the CPT® code’s Local Coverage Determination [...] - Reader Question:
Distinguish Between TV/TA Ultrasounds in Technique, Findings
Question: Do transvaginal and transabdominal ultrasounds (US) performed at the same encounter need to be separated [...] - Reader Question:
Go Unlisted For CAD With Breast US
Question: Which computer-aided detection (CAD) code should I use to report CAD with a breast [...] - Reader Question:
Be Wary of CT, Fluoro Guidance in Same Encounter
Question: I’m working on a fluoroscopic-guided lumbar puncture. At the beginning of the report, the radiologist [...]




