Upcoming Rulemaking: Prepare Now For Heavy Quality- Measure Scrutiny
Proposed rule will slash your reimbursement if you don’t report on these quality items.
All the talk about reporting standardized assessment data across post-acute care (PAC) settings is no longer just talk — the Centers for Medicare & Medicaid Services (CMS) announced a Notice of Proposed Rulemaking (NPRM) for the fiscal year (FY) 2016 SNF Prospective Payment System (PPS).
Tara McMullen, PhD, with the CMS Division of Chronic and Post Acute Care, detailed the proposed rule’s fine points in a May 14 SNF/LTC Open Door Forum (ODF).
Background: The FY 2016 SNF PPS proposed rule stems largely from the requirements contained in the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act), which includes SNF data submissions to CMS. The proposed rule applies to SNFs that meet the Medicare requirements for Part A coverage.
Get Ready to Report on These Areas
The IMPACT Act requires PAC providers, including SNFs, home health agencies, long-term care hospitals and independent rehab facilities, to report standardized assessment data on:
o Functional status;
o Cognitive function and mental status;
o Special services, treatments and interventions;
o Medical conditions and co-morbidities;
o Impairments; and
o Other categories.
o Functional status and changes in function;
o Cognitive function and changes in cognitive function;
o Skin integrity and changes in skin integrity;
o Medication reconciliation;
o Incidence of major falls;
o Transfer of health information when the individual transitions from the hospital/critical access hospital to PAC provider or home, or from PAC provider to another setting.
o Total estimated Medicare spending per beneficiary discharged to the community; and
o All condition risk-adjusted potentially presentable hospital readmission rates.
How Proposed Rule Affects Your Bottom Line
Take heed: Most important, beginning in FY 2018, SNFs that do not submit the required quality reporting data to CMS will have their annual payment update reduced by 2 percentage points, McMullen said. This is a 2-percent reduction to your FY 2018 market basket percentage.
Exception: The proposed rule does, however, allow a quality reporting program (QRP) submission exception and extension, which requires that you submit a written request within 90 days of the date extraordinary circumstances occurred.
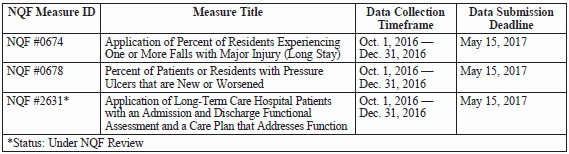
The proposed rule contains three proposed PAC cross-setting measures addressing skin integrity, major falls, and functional status and cognitive function.
Heads Up: Quality Measures Will Keep Coming
Look ahead: McMullen announced in the ODF possible additional quality measures for future consideration; these include:
In the ODF, McMullen also detailed the following considerations for meeting the October 2016 implementation date for the measure domains:
CMS accepted comments on the proposed rule until June 19. Stay tuned to future issues of MDS Alert for updates on changes to the proposed rule and the pending publication of a final rule.
Resource: The text of the proposed rule is available at www.federalregister.gov/articles/2015/04/20/2015-08944/medicare-program-prospective-payment-system-and-consolidated-billing-for-skilled-nursing-facilities. Also, you can access more information regarding the IMPACT Act at www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014-and-Cross-Setting-Measures.html.