Make Sure Your Turning/Repositioning Program Meets Surveyors' Expectations
Heed the RAI Manual’s instructions when coding M1200C.
You can employ a myriad of treatments and preventive measures when it comes to dreaded pressure ulcers, one of which is a turning/repositioning program. But is your turning/repositioning program up to snuff?
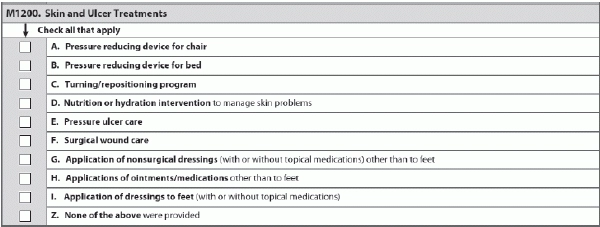
Turning/repositioning program (M1200C) is one of the various choices in Item M1200 — Skin and Ulcer Treatments. In this item, you check all that apply in the seven-day look-back period.
Key: Individualize Each Resident’s Program
To check M1200C for a turning/repositioning program, you must have specific approaches for changing a resident’s position and realigning his body, according to a recent presentation by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS). The medical record should include documentation that specifies intervention and frequency.
“This item on the MDS represents a critical intervention to prevent and heal pressure ulcers,” stressed MDS expert Judy Wilhide Brandt, RN, BA, RAC-MT, C-NE of Judy Wilhide Consulting Inc. in a June 8 analysis for Washington, D.C.-based Leading Age. “If a resident is at risk and does not have this intervention coded on the MDS, it is a matter of concern.”
The RAI Manual provides two tips for coding a turning/repositioning program under M1200C:
Important: If “every two hours” is a routine facility policy, it does not meet the criteria described in Section M of the RAI Manual to code for a turning/repositioning program, warns Marilyn Mines, RN, BC, RAC-CT, MDS Alert consulting editor and senior manager of clinical services for FROST Healthcare in Deerfield, Ill. The schedule must be specific to the resident’s needs, not facility policy.
Also, Example 4 on page M-42 in Section M clearly indicates that you must have an assessment/reassessment and documentation of the resident’s response to the turning and position, Mines adds.
Strategy: “A careful individualized assessment is the key to a successful program,” Brandt noted. “If the resident spends most of the time out of bed, for example, then off-loading while in the chair becomes critical.”
Repositioning an elder every two hours is alright if that’s what he needs, Boltz said. But you will find some residents who need repositioning more frequently to prevent redness.
This is why individualizing residents’ repositioning schedule is so important, Boltz stressed. You should also perform a tissue tolerance test to determine the right repositioning schedule for each resident.
What Surveyors Look For
Watch out: For instance, surveyors have specific guidance in the State Operation Manual for investigating a facility pressure ulcer prevention program. Surveyors are specifically assessing the following repositioning issues:
Except in rare cases, such as both sacral and ischial pressure ulcers are present, staff should not place a resident directly on the greater trochanter for more than momentary placement. Also, beware that elevating the head of the bed or the back of a reclining chair at or above a 30-degree angle creates pressure comparable to sitting and requires the same considerations regarding repositioning as for a dependent resident who is sitting.
Consider postural alignment, weight distribution, sitting balance and stability, and pressure redistribution when positioning a resident in a chair. Staff should teach residents to shift their weight approximately every 15 minutes while sitting in a chair.
Beware: Even though staff might report that a resident does have an effective turning/repositioning program, you still must have sufficient documentation to support your MDS coding, Brandt cautioned. If you don’t have sufficient documentation, “nurse managers should be notified so they can take credit for this very important intervention in the medical record.