Urology Coding Alert
Reader Questions:
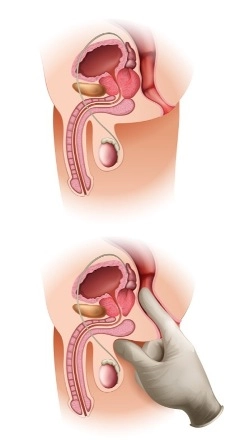
Use Caution on Post-Procedure Cath Removal Coding
Published on Fri Nov 11, 2022

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Urology Coding Alert
- In-office Testing:
Pinpoint Accurate Urodynamics Codes Based on Key Documentation Terms
Plus: Discover when reporting a separate E/M is possible. When patients present with urinary incontinence [...] - ICD-10-CM 2023:
Unlock SDoH Coding Success With These 6 FAQs
Look beyond the codes to the guidelines for all the info you need. On October [...] - News You Can Use:
Get the Details on Medicare’s 1-Year Split/Shared Policy Implementation Delay
You still have time to send feedback that could affect final changes. In the article, [...] - You Be the Coder:
Skip Coding Repair of Injuries Your Provider Caused
Question: My urologist states that a patient was scheduled for a penile prosthesis. However, due to [...] - Reader Questions:
Always Stress Documentation Requirements
Question: My provider looked to another provider for their opinion on one of our patient’s edema. [...] - Reader Questions:
Use Caution on Post-Procedure Cath Removal Coding
Question: The NCCI Policy Manual, Chapter XIII, Category III Codes makes the following reference to the [...] - Reader Questions:
Don’t Miss on Record Reviews
Question: How concerned should we be about medical record reviews by the Centers for Medicare & [...]
View All