Pinpoint Accurate Urodynamics Codes Based on Key Documentation Terms
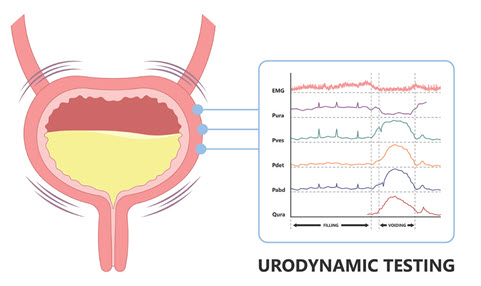
Plus: Discover when reporting a separate E/M is possible. When patients present with urinary incontinence or other symptoms affecting the urinary tract, your urologist may perform urodynamics tests, which evaluate how well the bladder can hold and empty urine. Because no single code covers every urodynamics test that your provider may perform, coding can be confusing when you encounter these tests in the urologist’s documentation. Consider these expert tips so you can more effectively report urodynamics codes accurately every time. Know the Terminology Differences Because you’ll find multiple CPT® codes that describe urodynamics, it’s important to understand how to link the terminology your urologist uses with the most accurate codes. Consider this guide to help you match the two: CMG: If the urologist documents a cystometrogram or CMG, that means they evaluated bladder capacity and pressures. You have two codes you can report: Urethral pressure profile studies: During these tests, the urologist measures resting and dynamic pressures in the urethral region that controls continence. You’ll report this service with 51727 (… with urethral pressure profile studies (ie, urethral closure pressure profile), any technique). In the urologist’s notes, you may see this described as a UPP. Keep in mind that some payers only allow you to collect for this test if previous tests have been inconclusive, so it’s essential to contact your insurer before administering a UPP study. Voiding pressure studies: If the urologist performs voiding pressure studies, they’re evaluating whether the patient can actually void their bladder appropriately (often to determine whether the patient has an obstruction). To report this service, you’ll submit one of the following codes: The only way you can choose between these two codes is to note whether the physician performs a urethral pressure profile study along with the voiding pressure study, so stress the importance of thorough documentation with your urologist. Because 51728 pays about $383 and 51729 reimburses approximately $405 (based on the 2022 national conversion factor), every instance of incomplete documentation could cost about $22. Make Sure the Documentation Includes These Specs Once you’ve pinpointed the most accurate code for urodynamics testing, your next step is to ensure that the documentation is thorough enough for the insurer. “Physician documentation is essential to determine what testing has been performed and including the test results supports the technical component of the procedure. A summary of each of these test results supports the professional component of the CPT® codes as well,” says Stephanie Stinchcomb Storck, CPC, CPMA, CCS-P, ACS-UR, longtime urology coder and consultant in Glen Burnie, Maryland. According to the Centers for Medicare & Medicaid Services (CMS) policy for urodynamics testing, that means the patient’s medical record must include: Other payers have even more specific rules in place regarding when urodynamic testing is payable. For instance, Blue Cross Blue Shield of Alabama says in its policy, which was updated in 2022, “for these studies to be covered, urodynamic testing and the interpretation of the tests must be done in the office, clinic, or facility of a participating provider and, if sent elsewhere for interpretation, be interpreted by a participating provider.” You should keep the test interpretation in the patient’s files, along with any printed images or tracings resulting from the tests. Know When Separate E/M Is Billable The National Correct Coding Initiative (NCCI) bundles the office/outpatient evaluation and management (E/M) codes (99202-99215) into the urodynamics testing codes. However, in some cases you may be able to report both, as long as your documentation supports a separately identifiable and significant E/M service. If so, you should append modifier 25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service) to the E/M code you report. E/M allowed: A patient presents to your practice complaining of incontinence. The urologist performs a full evaluation and then decides to administer a simple CMG test during the same visit. In this case, you should be able to report 51725 and the E/M code, with modifier 25 appended to the E/M. E/M allowed: A patient undergoes urodynamics testing, and then returns to the physician to collect the results a week later. During the subsequent visit, the urologist does not change or start a new treatment plan and the patient has no new complaints. Instead, the urologist only shares the results from the test. In this case, you should can report a separate E/M code, Storck advises. E/M not allowed: If a patient is scheduled for a urodynamics test only and there is no other interaction with the clinical provider, you cannot report a separate E/M code.