Urology Coding Alert
Compliance:
Assess CERT Findings to Identify Your Risk Areas
Published on Thu Apr 13, 2023

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Urology Coding Alert
- ICD-10-CM:
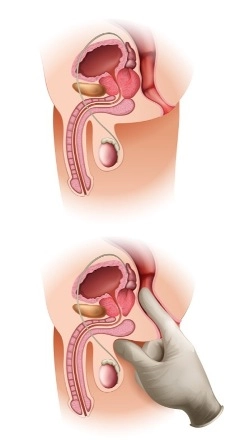
Master a Few Anatomic Terms to Ace Incontinence Coding
Master a Few Anatomic Terms to Ace Incontinence Coding Hint: Stress incontinence and overactive bladder [...] - Compliance:
Assess CERT Findings to Identify Your Risk Areas
Documentation improvement remains a key area on which you should focus. Knowing where to focus [...] - Artificial Intelligence:
Let AMA’s AI Classifications Guide Your Learning
Not all AI is created equal, and knowing the nuances will affect your code categorization. [...] - You Be the Coder:
Test Your Biopsy Imaging Know-How
Question: How would I report the procedure described in this operative report? There is also an [...] - Reader Questions:
CMS Isn’t Fooling You With These April 1 ICD-10 Updates
Question: Have new codes been recently added to ICD-10-CM? I thought new codes only came into [...] - Reader Questions:
Don’t Automatically Use NCCI to Override a Bundle
Question: I have a physician who keeps wanting to bill 52356 and 52352 together on the [...]
View All