Will Radiology Practices Face Another Year of Medicare Cuts?
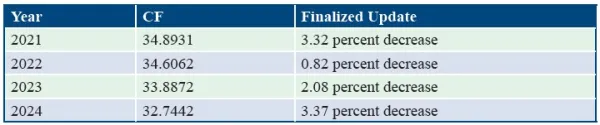
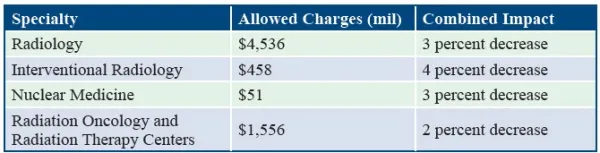
Plus: Learn which codes receive refined RVUs. On Nov. 16, 2023, the Centers for Medicare & Medicaid Services (CMS) published the calendar year (CY) 2024 Medicare Physician Fee Schedule (MPFS) final rule to the Federal Register, and once again, radiology practices face reduced reimbursement rates for the upcoming year. Find out what else CMS has in store for radiology practices in 2024. Prepare for a 4th Straight Year of Reduced CF In the CY 2024 MPFS, CMS announced a conversion factor of $32.74, which marks a fourth straight year of decreased conversion factors (CF). The 2024 CF is a $1.15 reduction — or a 3.37 percent decrease — from the 2023 MPFS CF. CMS last approved an increased CF for CY 2020, and each year since has resulted in a decreased CF: CMS calculated the 2024 MPFS CF using the following factors: Last year’s Consolidated Appropriations Act (CAA) legislation provided a 2.5 percent increase for the CY 2023 CF to offset the reduction, but Congress authorized only a 1.25 percent increase for CY 2024. The impact of this CF decrease will be felt by several specialties, including radiology. Each radiology-related specialty will see an estimated combined impact of at least -2 percent in 2024: The impact table doesn’t include any changes to the CF as a result of the CAA payment supplements for 2024. “The actual impact on specialties would be approximately 1.25 percent lower,” wrote McDermott+Consulting, an affiliate of law firm McDermott Will & Emery, in a rule summary (www.mcdermottplus.com/insights/cms-releases-cy-2024-physician-fee-schedule-final-rule/). The MPFS also confirms a Medicare Economic Index (MEI) increase of 4.6 percent for 2024, which is an increase over 2023’s 3.8 percent. The MEI is a formula used to ensure Medicare reimbursement rates keep up with medical care costs and inflation. CMS calculated the 2024 MEI as the “most recent historical percentage increase of the 2017-based MEI reflecting historical data through for the second quarter of 2023,” the Agency writes in the MPFS final rule. Reactions to the Economic News Professional healthcare organizations met the news of a CF reduction and an MEI increase with disappointment. “This is a recipe for financial instability,” says Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association (AMA). “The declining revenues in the face of steep cost increases disproportionately affect small, independent, and rural physician practices, as well as those treating low-income or other historically minoritized or marginalized patient communities” (www.ama-assn.org/press-center/press-releases/medicare-payment-cuts-thin-gruel-seniors-physicians). Radiologic societies were also displeased with the reduced reimbursement rates. “[The] American Society for Radiation Oncology (ASTRO) is deeply disappointed that CMS finalized an additional 2 percent cut to reimbursement for radiation therapy in today’s MPFS final rule. The consistent decline in Medicare reimbursement for radiation oncology threatens to undermine patients’ access to vital cancer care across the country,” says Jeff M. Michalski, MD, MBA, FASTRO, chair of the ASTRO board of directors (www.astro.org/News-and-Publications/News-and-Media-Center/News-Releases/2023/Medicare-physician-payment-final-rule-cements-more). ASTRO is requesting Congress to intervene with legislation that helps stabilize reimbursement in the short term while also ensuring “long-term viability” for radiation oncology. Prepare for an Indefinite Pause to the AUC Program CMS is finalizing pausing the Protecting Access to Medicare Act (PAMA) Appropriate Use Criteria (AUC) program for advanced diagnostic imaging. Citing implementation issues, CMS is choosing to pause the program to reassess it, and the agency is also ceasing the existing educational and operations testing period. The Agency believes the real-time, claims-based reporting requirement “presents an insurmountable barrier for CMS to fully operationalize the AUC program.” Examine Finalized RVUs for Radiology Codes CMS finalized the work relative value units (RVUs) of certain radiology codes as recommended by the Relative Value of Service Update Committee (RUC). CMS is finalizing a work RVU of 0.30 and the direct practice expense (PE) inputs for +76937 (Ultrasound guidance for vascular access requiring ultrasound evaluation of potential access sites, documentation of selected vessel patency, concurrent realtime ultrasound visualization of vascular needle entry, with permanent recording and reporting (List separately in addition to code for primary procedure)). Code 27278 (Arthrodesis, sacroiliac joint, percutaneous, with image guidance, including placement of intra-articular implant(s) (eg, bone allograft[s], synthetic device[s]), without placement of transfixation device) is a new addition to the CPT® code set in 2024. CMS is finalizing a work RVU of 7.86, as well as the proposed direct PE inputs. Another addition to the 2024 CPT® code set is 75580 (Noninvasive estimate of coronary fractional flow reserve (FFR) derived from augmentative software analysis of the data set from a coronary computed tomography angiography, with interpretation and report by a physician or other qualified health care professional). The CPT® Editorial Panel approved this code “to report a non-invasive estimate of coronary fractional flow reserve derived from augmentative software analysis of the dataset from a coronary computed tomography angiography,” CMS writes in the final rule. CMS is also finalizing the direct practice expense (PE) refinements for neuromuscular ultrasound codes 76881-76883. Review the CY 2024 MPFS Final Rule in the Federal Register here: www.federalregister.gov/public-inspection/2023-24184/medicare-and-medicaid-programs-calendar-year-2024-payment-policies-under-the-physician-fee-schedule.