Review Codes For Percutaneous Biliary Interventions and Radiological Assistance
Codes include imaging guidance and radiological supervision.
In the past few issues of Radiology Coding Alert, we have been reviewing the 2016 reforms. It is now time to check if you have embraced the coding for biliary interventions that has been revamped this year. Of particular interest to your practice are the services of your radiologist in the percutaneous biliary procedures. In 2016, there have been additions of three new codes for percutaneous biliary stenting. Here is a quick guide to confirm if your practice has aligned to the new codes.
Tip 1: Check if you included three new codes in your list
CPT® 2016 deleted code 47511 (Introduction of percutaneous transhepatic stent for internal and external biliary drainage) — the only code you ever had for percutaneous biliary stenting — and replaced it with the following three codes:
Radiological assistance: The new codes are inclusive of radiological assistance, fluoroscopy and ultrasound.
How to choose the right code? To choose between these codes, you “need to know if it’s a new access or going through a tube already in place,” according to AMA CPT® editorial panel member Katharine L. Krol, MD, FSIR, FACR at the AMA’s CPT® and RBRVS 2016 Annual Symposium. That allows you to choose between 47538 for existing access, or one of the other codes for de novo access.
You should also answer the question, “Is the cath left in place afterwards or did we just put a stent in and then abandon access?” according to Krol. That allows you to choose between 47539 and 47540.
Tip 2: ‘Catheter’ and ‘Stent’ aren’t the same
You (and also your provider) may have used the words “catheter” and “stent” somewhat interchangeably. However, the CPT® codes are specific. You need to be very clear if your physician’s services included a stent or a catheter.
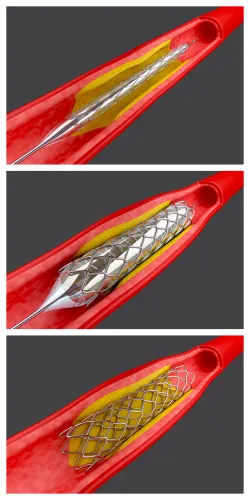
“The biliary stent can have a couple of different configurations,” Krol says. “You can have stents that look like stents you put in a blood vessel,” such as metallic expanding stents. Or you may have plastic “catheter types that are all internal, and those are also called stents and reported with stent codes as defined by CPT®,” according to Krol.
On the other hand, percutaneous biliary catheters always have external accessibility for drainage. “It can be either an external biliary drain or an inter-anal-external biliary drain, but the point is that the catheter sticks out of the patient,” Krol says. You should not report percutaneous biliary catheter procedures with the stent codes, but should turn instead to new codes 47533 (Placement of biliary drainage catheter, percutaneous, including diagnostic cholangiography when performed, imaging guidance [e.g., ultrasound and/or fluoroscopy], and all associated radiological supervision and interpretation; external) - 47537 (Removal of biliary drainage catheter, percutaneous, requiring fluoroscopic guidance [e.g., with concurrent indwelling biliary stents], including diagnostic cholangiography when performed, imaging guidance [e.g., fluoroscopy], and all associated radiological supervision and interpretation). The radiological supervision and imaging guidance services of your radiologist are covered in these codes.
Key: Stents are “totally internal, not externally accessible,” Krol emphasizes. Even if the op report calls a catheter with an external drain a stent, you should not use the stent codes.
Tip 3: You shouldn’t always code for each stent
For the most part, you shouldn’t code for each stent. Instead, you should report these codes once per session for a single bile duct or a single lesion that crosses more than one bile duct. You may like to check if your physician used a single percutaneous access.
“One thing about the stent codes that I noticed is that the code nomenclature still says ‘each stent,’ but there is a lot of introductory language telling you that isn’t the case,” Krol says.
The CPT® section introduction states, “Codes 47538, 47539, 47540 may be reported only once per session to describe one or more overlapping or serial stent(s) placed within a single bile duct, or bridging more than one ductal segment (e.g., left hepatic duct and common bile duct) through a single percutaneous access.”
In other words, the unit of service “is not each stent,” Krol says.
Caveat: Sometimes you can report multiple percutaneous biliary stent codes for the same patient on the same day, such as the following circumstances:
Check modifiers: If your physician documents one of these conditions, you can report multiple stent codes for a single session and append modifier 59 (Distinct procedural service) or similar modifier to the additional stent codes.
Tip 4: Find where bundling can restrict
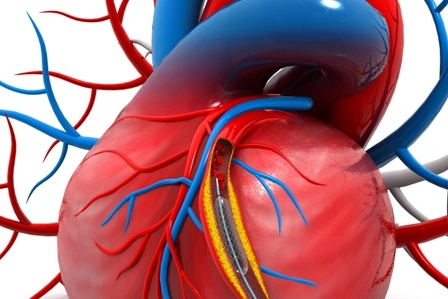
One of the primary reasons for this section update in CPT® 2016 is to bundle imaging services with the surgical procedures. That means all of the new percutaneous biliary procedure codes, including 47538-47540, incorporate imaging guidance such as fluoroscopy or ultrasound, and radiological supervision and interpretation (S&I). The procedures also include diagnostic cholangiography, balloon dilation, and catheter exchange or removal, if performed.
That leads to a host of code bundles that CPT® notes in the text, such as the following:
Nor should you report the percutaneous stent codes with codes for similar procedures through the same access, or biliary procedures that utilize a different approach, such as endoscopic. That’s why CPT® provides the following notes: