Radiology Coding Alert
CPT® 101:
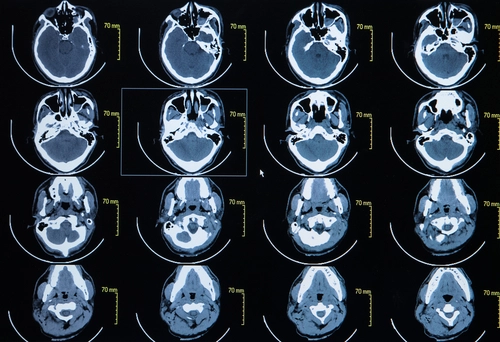
Avoid Going to Extremes When Coding Arm and Leg CTAs
Published on Thu Mar 23, 2023

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Radiology Coding Alert
- CPT® 101:
Avoid Going to Extremes When Coding Arm and Leg CTAs
Learn if contrast is required to report 73206 or 73706. Providers order computed tomography angiography [...] - Case Study:
Identify Key Terms in This Renal Duplex Scan Imaging Report
Will you need to modify your renal scan code choices? Find out. Choosing the correct [...] - Modifier Mania:
Find Answers to Your Laterality Modifier FAQs
When in doubt, prompt the payer for their preferences. The CPT® code set is packed [...] - You Be the Coder:
Choose the Correct Code for a Prostate MRI
Question: I have a report that indicates a radiologist performed magnetic resonance imaging (MRI) of a [...] - Reader Questions:
Report an I&D With a Facial CT Scan
Question: After a CT maxillofacial scan without contrast, our radiologist performed and incision and drainage of [...] - Reader Questions:
Skip Two Unilateral Codes When a Bilateral Code Exists
Question: We had a report that indicated the provider performed X-rays of both of the patient’s [...] - Reader Questions:
Double-Check Descriptors to Avoid Duplicate Guidance Billing
Question: A physician in our outpatient clinic performed an US-guided core needle biopsy of an axillary [...] - Reader Questions:
Examine This Explanation Between Excludes1 and Excludes2 Notes
Question: I’m new to medical coding, and the ICD-10-CM Official Guidelines regarding Excludes1 and Excludes2 notes [...]
View All