Avoid These 5 Deadly Mistakes for Lung Cancer Screening Claims
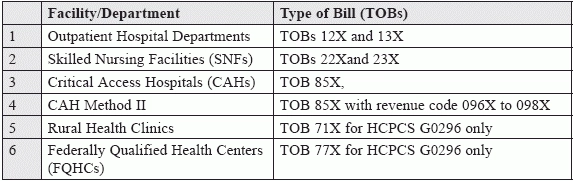
Use the right TOBs, and avoid facing claim adjustments. CMS now provides coverage for screening for lung cancer with LDCT, and you have two new HCPCS codes G0296 (Counseling visit to discuss need for lung cancer screening [LDCT] using low dose CT scan [service is for eligibility determination and shared decision making) and G0297 (Low dose CT scan [LDCT] for lung cancer screening), to report a shared decision making visit for screening for lung cancer. "With the focus on prevention, this adds to the array of tools the physician has to provide for quality care and early detection," says Carol Pohlig, BSN, RN, CPC, ACS, senior coding and education specialist at the Hospital of the University of Pennsylvania. Apart from the basic information on eligibility and billing requirements, which you can find in the last issue's article "Tread Cautiously with the New LDCT Lung Cancer Screening SDM Reporting" in Pulmonology Coding Alert, Volume 17, Number 6, you must also know about the claim requirements, as well how to decipher the denial codes. Read on to know more. Know the Type of Bills to Use Starting the institutional claim with the correct form is the most important step you can take to ensure successful payment of your claims. Medicare has identified acceptable service locations with different types of bills that are facility specific. You may use these for claims for lung cancer screening codes G0296 and G0297, dated for services rendered Feb. 5, 2015, onwards. Medicare will pay for the services according to the type of facility or department where the services are provided: "We have a check list that we go through on each patient when we schedule this test. A radiology representative calls the pulmonology nurse and they go through all of the criteria together," reveals Lisa Center, CPC, Physician Practice Manager at Via Christi Hospital Pittsburg, Inc., in Pittsburg, Ks. Avoid These Mistakes That May Lead to Claim Adjustments If you did not document your claim properly, get ready to receive denials with codes such as Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes (RARCs), and Group Codes. Here are the top five mistakes to watch for so you'll have fewer problems. 1) Always Use an Appropriate TOB: If you did not use a type of bill (TOB) appropriate to your facility, here is what you may expect from Medicare: That's not all. You may also see a Group Code CO (Contractual Obligation), putting the financial onus on you, as a provider, in case you billed the claim with a GZ modifier (Item or service expected to be denied as not reasonable and necessary), with no ABN (advance beneficiary notice) in the patient's file. In this case you may also expect a CARC 50 code. 2) Do Not Bill G0296 with Another Same Day Service in Certain Locations: When using TOBs 71X and 77X, do not commit this mistake, unless you are conducting an initial preventive examination. Here are the codes that Medicare may slam you with in such a case: "I would use a modifier 25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service), if I did an E/M in addition to this screening counseling," says Center. 3) Do Not Re-Bill G0297 within a Year: You may be questioned, and denied payment, if you ask for additional G0297 reimbursement too soon. As per the coverage criteria, you can bill G0297 for a specific patient not more than once in a year. Keep in mind that at least 11 months must have gone by since the last screening. Denial codes to expect are: 4) Double Check the Patient's Age: You may lose your deserved money for all your hard work on the patient on the shared decision making visit, just because the patient does not fall into the requisite age range of 55 to 77 years, at the time of counseling. 5) Never Miss the ICD-10 Diagnosis Z87.891: Make sure your claims carry the time appropriate diagnosis V15.82 (Personal history of tobacco use) for claims prior to Oct.1 2015, and Z87.891 (Personal history of nicotine dependence) for claims for services on or after Oct. 1, 2015. If you miss that, here is what you may get from Medicare: Final takeaway: "The claims have just started to be processed, and there is no data base for this code just yet," admits Pohlig. You will need to draw your own strategy, and try not to commit the mistakes Medicare has already warned you about. "My advice would be to work closely with your pulmonologist and radiology department to come up with a checklist so that you ensure that all of your tests follow the criteria," advises Center.