Pulmonology Coding Alert
Answer 4 Questions to Crank Up Your Critical Care Payouts
Don’t give up deserved payment for unbundled services along with critical care.
If you have struggled in the past to get paid for justified critical care (CC) services provided by your pulmonologist, you may not be actually taking care to tick the right boxes on critical points. Answer these questions to unlock theCCreimbursement potential successfully.
1. Is Uncertain Admission Status Sinking Your Claim?
Do not jump on every chance to select CC codes 99291 (Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74 minutes) and +99292 (Critical care, evaluation and management of the critically ill or critically injured patient; each additional 30 minutes [List separately in addition to code for primary service]) whenever your pulmonologist provides CC services. Keep your eyes peeled to catch relevant indicators in the physician’s notes that justify CC to the patient.
CMS has strict rules regarding family counseling time and coding for concurrent critical care and you should adhere to them before reporting these two codes. Relevant points include verifying that “the patient is critically ill, which requires that the patient have at least one organ system that is failing and that the patient’s life is in jeopardy.” CMS adds that in order to qualify as CC for Medicare patients, “the failure to initiate these interventions on an urgent basis would likely result in sudden, clinically significant or life threatening deterioration in the patient’s condition.”
According to CPT®, CC services are defined as a physician’s direct administration of medical care to a critically ill or critically injured patient and involves decision making of high complexity to assess, manipulate, and support vital organ system failure and/or to prevent further life threatening deterioration of the patient’s condition.
Stop: If a patient is in the intensive care unit (ICU), that does not automatically qualify him as critical and, by the same logic, not all critical cases will be found only in the ICU. The key indicator is the high degree of chance that the patient may face an imminent and life-threatening deterioration with respect to the condition you are managing (as opposed to conditions managed by other specialists).
2. Is Time On Your Side?
Remember that “calendar day” is the pivotal unit of measuring service in CC parlance. “The rule is from midnight to midnight (one calendar day),” says Carol Pohlig, BSN, RN, CPC, ACS, Senior Coding & Education Specialist at the Hospital of the University of Pennsylvania.“You cannot carry over any CC time any time on Day 2. If your services have been performed continuously on Day 1 and have carried over at midnight into Day 2, then you should only report the time before midnight of Day 1 as critical time given,” she adds.
For example, an unconscious patient is brought into the emergency department (ED) at 11.15 p.m. of Day 1 with respiratory failure caused by chronic obstructive pulmonary disease (COPD). The ED physician calls in the pulmonologist, who immediately orders an arterial blood gas (ABG) study that reveals respiratory acidosis. The pulmonologist then proceeds to insert an endotracheal tube and places the patient on a ventilator. The pulmonologist notes in the chart that the patient is critically ill and monitors his condition for about 50 minutes until 12.05 a.m. of Day 2 when the patient stabilizes.
Count the minutes: “The five minutes (12:00 -12:05) on Day 2 would not be included in the critical care time for Day 1, and you could not bill a separate E/M for it since it was part of Day 1. The 5 minutes would count towards the cumulative CC time, as long as you spend >30 minutes of critical care on Day 2,” informs Pohlig. In this case you will be able to report 99291 only once for Day 1. The coding rules will remain the same even if the respective times were far from midnight.
A physician’s time for CC services includes the time spent engaged in direct care of the individual patient at the bedside as well as elsewhere on the unit/floor. For example, the pulmonologist may be reviewing test results, analyzing the case with support staff, updating her medical documentation, or giving counseling time to family members.
It is not necessary that the time is continuous, but you should ensure that the physician diligently recorded her activities during her charge as critical care provider. However, the time provided by the pulmonologist must be within the unit/floor as the patient and she should be immediately available for the patient.
Here’s another example: Your pulmonologist provided 60 minutes of critical care to stabilize a patient at 10 a.m. Around noon, the nurse again called the physician as the patient’s condition had worsened. She provided another 30 minutes of critical care. Even though the service time blocks were not contiguous, you can still report the totalcritical care time.You can report:
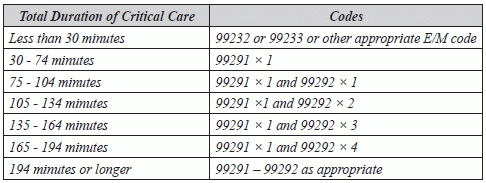
You can follow the time chart CMS has provided as a guide for critical care reporting:
3. Have You Provided Other Services With CC?
If you think that CC codes are all-encompassing and you can’t bill other services that your pulmonologist provided on the same day as critical care, then you are losing out on major dollars. You have to be careful about the ones to omit from the claim. You cannot report services such as:
“Once critical care services are required upon the patient’s presentation to the hospital emergency department, your pulmonologist cannot code separately for services such as an initial emergency department E/M (99281-99285, New or Established Patient Emergency Department Services) for patients, cautions Pohlig. “Once critical care is initiated, youcannot bill any other E/M service that day,” she adds.
However, you can bill for unbundled services such as:
You can also bill for initial or subsequent hospital care services for the same day as CC, if the patient was seen prior to requiring critical care services.
For example: The physician sees an inpatient in the morning and provides hospital care. Then, in the afternoon, the patient’s condition worsens dramatically and the physician provides critical care services. In this instance, you can bill for both the critical care services and the initial hospital care service (99221-99223). Remember to append modifier 25 (Significant, separately identifiable evaluation and management service bythe same physician or other qualified health care professional on the same day of the procedure or other service) to the initial hospital care service to indicate that it was significant and separately identifiable from the critical care service.
So, in this scenario, for example, if the physician provides moderately complex initial care for 50 min. in the morning and then critical care for 30 min. in the afternoon, you would code:
Caution: Do not add the time spent on the initial service (i.e., 99222) to the cumulative critical care time. Be sure to correctly date and time each encounter. Documentation will be requested by the payers so that they can review the “timeline” of services, ensuring that the critical care was not required until later in the day.
4. Has Your Documentation Kept Up With Your Services?
Critical care is commonly performed but underreported. Many physicians often miss critical care coding opportunities. Before submitting the final claim for services that are considered critical care, check the physician’s notes to see:
Once you’ve answered these questions, you can determine whether reporting for critical care services is appropriate.
Pulmonology Coding Alert
- Critical Care:
Answer 4 Questions to Crank Up Your Critical Care Payouts
Don’t give up deserved payment for unbundled services along with critical care. If you have [...] - Modifier Alert:
Distinguish Between Modifiers 52 and 53 to Avoid Denials
Voluntary termination of procedure by the patient does not count. When your pulmonologist curtails or [...] - Consultation Coding:
Capture Deserved Consult Payment With These Tips
Codes 99241-99245 are still viable in some cases. If your pulmonologist provided an office consultation [...] - Readers Query:
Sound Out Your Payer Before Billing ANS Testing
Question: Our office just came across a case of ANS testing. Is it a payable [...] - Reader Query:
Check CCI Edits For Final Say on Spirometry Bundles
Question: I am going to bill 94150 and 94726. The CCI edits do not show the [...] - Reader Query:
Safely Report Critical Care and Consult On the Same Day
Question: We recently had this type of claim. Hospital Consultation/ (High Complexity), Critical Care First Hr., [...] - You Be the Coder:
Press the Pause Button Before Billing Oximetry and E/M Together
Question:We are billing an evaluation and management (E/M) code 99212 along with a pulse oximetry [...]

