4 Tips Will Perfect Your Psychoactive Substance Use Behavioral Disorder Claims
Hint: Watch provider documentation to zero in on the right code.
When your psychiatrist arrives at a diagnosis of behavioral disorder due to psychoactive substance use, you will need to carefully look through patient documentation to identify the type of substance the patient is using, the extent of usage, and the type of behavioral problems the patient is experiencing. This will help you zero in on the right diagnosis code to report for the particular patient.
Use these four expert tips to guide you through reporting of behavioral disorder due to psychoactive substance abuse.
Tip 1: Get Started With Recognizing Substance Type
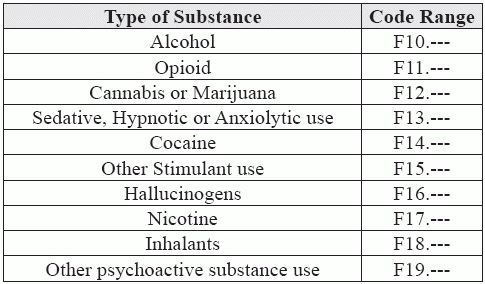
When your clinician diagnoses a behavioral disorder due to psychoactive substance use, you will begin your ICD-10 code selection by looking at the code range F10-F19. “Codes are classified by the type of substance (such as sedative, cocaine, alcohol, nicotine, hallucinogen, other stimulant, etc.) and whether the disorder is use, abuse, or dependence,” says Lorraine M. Papazian-Boyce, MS, CPC, AHIMA-Approved ICD-10-CM/PCS Trainer, President of PB Resources, Inc. in Belfair, WA.
You can keep the following chart handy to help you quickly identify the code range you will need to report depending on the type of substance the patient is using.
So, first, you need to identify the type of psychoactive substance the person is using to select the appropriate section of codes. For instance, if the patient is diagnosed with behavioral disorder due to cannabis use, you will have to report an appropriate code from the F12.--- (Cannabis related disorders) set of codes.
Tip 2: Discern Between Abuse and Dependence
Once the appropriate code set is identified, you will need to look at patient documentation to check the extent of use of the psychoactive substance. You will need to look at the chart notes to see if your clinician has identified the extent of use as “abuse” or “dependence.” “Coding of abuse or dependence must be based on provider documentation,” Papazian-Boyce asserts. If your clinician has not mentioned the extent of usage, you will need to identify it from patient documentation or query your clinician. “Report the “unspecified” set of codes only if absolutely necessary, because insurance companies often require the most specific code available to consider reimbursement,” Papazian-Boyce adds.
“Abuse is using the substance in a quantity or with a frequency that it creates life problems such as legal, employment, social, or family issues. It might place the person at physical risk without causing physical dependence,” Papazian-Boyce says. “Dependence, also called addiction, is a compulsive physical or psychological reliance on the substance to a degree that attempting to stop creates physical symptoms of withdrawal.”
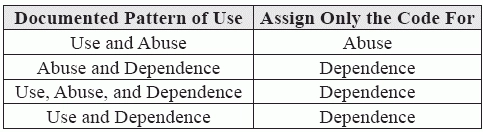
Sometimes, provider documentation may refer to use, abuse, and dependence of the same substance (e.g., alcohol, opioid, cannabis, etc.). In this situation, per ICD-10-CM guidelines, only one code should be assigned to identify the pattern of use based on the following hierarchy:
You can keep the following table provided by Melody Lidmila, CPC, CEC, coding specialist at the University of Colorado Health, in Loveland, CO handy to easily identify from patient documentation about whether to use “abuse” or “dependence.”
“In essence, ICD-10-CM guidelines create a hierarchy of use with ‘use’ on the low end, ‘dependence’ on the high end, and ‘abuse’ in between,” says Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians. “Per the guidelines, you should code the highest level of use documented.”
Tip 3: Look for Complications
Once you have identified the extent of usage, you will need to check patient documentation to identify the “complications,” if any, that the patient is experiencing to zero in on the code to report for the particular diagnosis. “Identify the correct specifiers and add the appropriate code extension. For example, is it uncomplicated, with intoxication, in remission, etc.,” Lidmila says. You will need to look through patient documentation to see if your clinician has identified complications like intoxication, delirium, perceptual disturbance, delusions, hallucinations, anxiety, etc.
For instance, if your clinician has diagnosed the patient with “cannabis abuse with intoxication,” without any other complications, you will report F12.120 (Cannabis abuse with intoxication, uncomplicated). However, if he also reports that the patient is also experiencing “delirium,” you will have to report the diagnosis with F12.121 (Cannabis abuse with intoxication delirium).
Tip 4:Heed These Expert Additional Tips
Here are some additional pointers provided by Papazian-Boyce that will help you fine tune the reporting of behavioral disorders due to psychoactive substance use: