Breathe New Life Into “Simple” Bronchitis Coding
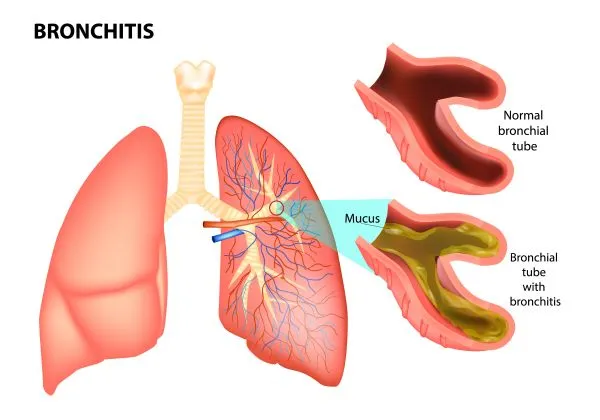
Also: see which Z codes could apply to your claim. Bronchitis is a common condition, and one that primary care practices see often. When the physician describes the condition as “simple,” sometimes the condition is anything but. For example, how can a simple condition also be chronic? Figuring out which code to choose can have you second-guessing yourself and wondering whether you need to query for more information. When the diagnosis is “simple,” we’re here to help you decipher which code to choose. Condition refresh: Bronchitis is the inflammation of the mucus membrane in the lungs and bronchial passages. The respiratory disease causes the irritated membrane to swell, get thicker, and narrow or close the airways. This can cause the patient to cough, experience shortness of breath, and expectorate the phlegm. Distinguish Between Acute and Chronic Acute: Patients typically develop acute bronchitis because of a viral infection. Acute bronchitis typically lasts for several weeks. Chronic: Chronic bronchitis is a condition where the patient experiences a cough and mucus most days for at least three months in a year, and for two consecutive years. Cigarette smoking is one of the main causes of chronic bronchitis, but several factors and comorbidities that contribute to the condition include: Patients with chronic bronchitis can experience an acute exacerbation of their chronic condition, which is diagnosed as acute on chronic bronchitis. Reminder: You’ll assign acute or chronic condition codes based on the provider’s documentation, since the ICD-10 code set doesn’t provide definitions for acute or chronic conditions. So, if the physician definitively diagnosis the patient as having bronchitis that is chronic, but also “simple,” which code set makes the most sense? Use the Alphabetic Index to Arrive at the J41.- Codes When you search for the conditions in the ICD-10 Alphabetic Index, you’ll look for Bronchitis > chronic > simple or Bronchitis > chronic > mucopurulent to direct you to the correct code choices in the Tabular List. Both listings direct you to the J41.- code category (Simple and mucopurulent chronic bronchitis), which features codes dedicated to simple bronchitis and mucopurulent bronchitis diagnoses. Here’s what each of those conditions entails. Simple chronic bronchitis: Patients suffering from simple chronic bronchitis, coded to J41.0 (Simple chronic bronchitis), experience frequent coughing with clear secretions. Patients with bronchitis may experience shortness of breath, but patients with simple chronic bronchitis do not, even though the bronchi are narrowed. Mucopurulent bronchitis: If the physician diagnoses the patient with mucopurulent chronic bronchitis, then you’ll assign J41.1 (Mucopurulent chronic bronchitis). “Mucopurulent chronic bronchitis is differentiated from simple chronic bronchitis in that mucopurulent bronchitis is a type of bronchitis that produces pus in addition to mucus,” says JoAnne Wolf, RHIT, CPC, CEMC, coding manager for Children’s Health Network in Edina, Minnesota. Sputum associated with mucopurulent chronic bronchitis may be described as somewhat thicker and cloudy or opaque in appearance. The sputum may also become darker with a hint of yellow or green if an infection causes sputum production. Note: It’s also possible for a patient to have simple and mucopurulent chronic bronchitis, which codes to J41.8 (Mixed simple and mucopurulent chronic bronchitis). Remember to Heed the Excludes Notes The alphabetic index should always lead you to the Tabular List, and once you’re there, be sure to not overlook the notes that offer specific coding instructions. For example, parent code J41.- features an Excludes2 note that enables you to assign J42 (Unspecified chronic bronchitis) or any of the J44.- (Other chronic obstructive pulmonary disease) codes for the conditions specified by the J41.- codes when the conditions coexist. “The Excludes2 note means ‘not included here’,” says Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians. An Excludes 2 note indicates that although the excluded condition is not part of the code family in question, a patient may have both conditions at the same time. So, when an Excludes 2 note appears under a code, you typically may use both the code and the excluded code together if supported by the medical documentation. “However, I would still not report J42 with any of the J41.- codes,” adds Moore, “because there is an Excludes1 note under J42 that references J41.-, and Excludes1 means the conditions are mutually exclusive.” Also: You’ll also need to assign tobacco-related codes if the provider’s documentation includes that information. “Because chronic bronchitis is most often caused by cigarette smoking, it is important to also code for tobacco dependence or use, exposure to tobacco smoke, or history of tobacco dependence,” Wolf says. You’ll assign one or more of the following codes to identify a patient’s involvement with tobacco: Practice Sound Sequencing Even if you’ve paid accurate attention to the Excludes notes, the payer may still reject your claim if the codes aren’t sequenced properly. Consider the following example: An established patient presents to your primary care practice with a cough that produces clear secretions and a discomfort in the chest. The patient has experienced the symptoms for several months. The patient currently smokes two packs of cigarettes a day and has failed to quit several times. After testing, the physician diagnoses the patient with simple chronic bronchitis. Coding: You’ll need to assign two ICD-10-CM codes for this scenario. First, you’ll assign J41.0 to report the simple chronic bronchitis diagnosis. Next, you’ll assign F17.210 (Nicotine dependence, cigarettes, uncomplicated) to report the patient’s cigarette smoking habit. The 5th character “1” indicates the patient’s dependence on cigarettes, and the 6th character “0” shows the patient’s inability to stop using cigarettes and that the condition isn’t complicated by other factors like cigarette withdrawal or other nicotine-induced disorders.