Hint: Pay attention to condition synonyms and procedure complexity.
If you revert to autopilot when it comes to coding pilonidal cysts, then you could be missing key details that will maximize your practice’s ethical reimbursement. Dig deeper with this scenario to make sure you capture all of your physician’s work.
Read This Scenario
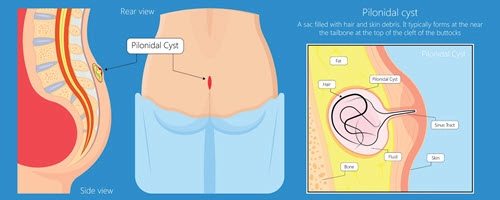
A patient reports to your provider with a swollen mass just above the cleft in his buttocks right around the coccyx. Pus is draining from the abscessed mass, and the area around it is red. After an examination of the mass, your provider numbs the area with 1 per cent xylocaine, then uses a 30-gauge needle and a #11 blade to drain the area of pus and remove caseous material. Your provider then packs and dresses the area and prescribes antibiotics for the patient.
How would you go about coding this encounter?
Decide Between Abscessed or No
On the surface, the diagnosis code for the patient’s condition seems relatively straightforward. The ICD-10 alphabetic index entry for Cyst – pilonidal directs you to L05.91 (Pilonidal cyst without abscess) for a pilonidal cyst that has not abscessed. Per the code synonyms, you could also use this code if the provider documented the cyst as a pilonidal or postanal dimple.
But this is not what the provider has documented in this scenario, as the note indicates that there is pus draining from the abscessed mass. In this case, the alphabetic index directs you to L05.01 (Pilonidal cyst with abscess), which the provider may also have documented with synonyms such as pilonidal abscess, pilonidal dimple with abscess, or postanal dimple with abscess.
However, several other complicating factors may prevent you from applying L05.01 as the correct diagnosis code in this situation. They involve clinical terminology that may require querying the provider to arrive at the most specific ICD-10 code possible.
Decide Between Cyst or Sinus
To make the correct decision in this choice, you must first make sure that the patient’s condition is a pilonidal cyst and not a pilonidal sinus, a similar condition but one that is distinguished by a small hole in the patient’s skin. This may also be referred to in the provider’s notes as coccygeal fistula or sinus or a pilonidal fistula and would be coded to L05.02 (Pilonidal sinus with abscess) if the fistula has abscessed, or L05.92 (Pilonidal sinus without abscess) if it hasn’t.
Last, you may also see a pilonidal cyst referred to as a sacrococcygeal cyst. So, you should code the conditions accordingly or seek clarification from your provider if you are unsure as to the correct coding.

Decide Between Simple or Complicated
Procedure coding for pilonidal cyst incision and drainage is, again, easy on the surface. That’s because CPT® has codes specific to the condition, enabling you to bypass incision and drainage (I&D) procedure codes 10060 (Incision and drainage of abscess [eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia]; simple or single) and 10061 (…complicated or multiple) for the more specific 10080 (Incision and drainage of pilonidal cyst;simple), or 10081 (Incision and drainage of pilonidal cyst; complicated).
But like your diagnosis code choice, you’ll have to make two critical decisions before you arrive at the correct code.
The first decision involves determining whether the I&D was simple or complicated, which is not as easy as it looks. That’s because “CPT® does not define ‘simple’ or ‘complicated’ in this context,” says Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians.
Why? “Per a Q&A that appeared in the December 2006 issue of CPT® Assistant (Volume 16, Issue 12), ‘the choice of code is at the physician’s discretion, based on the level of difficulty involved in the incision and drainage procedure,’” Moore adds.
So, to make the decision, you will either have to look closely at the provider’s note or query the provider directly.
Decide Between I&D, Excision
In some instances, a clinician might perform an I&D of a pilonidal cyst and then determine that an I&D will not help in completely eliminating the problem. So, the provider then performs an excision of the cyst at the same encounter. In such a case, you have three CPT® codes to report the excision of the pilonidal cyst: 11770 (Excision of pilonidal cyst or sinus; simple), 11771 (…extensive), or 11772 (…complicated).
Again, you will have to closely examine the provider’s note, or query the provider directly, to determine what they did and whether the procedure was simple, extensive, or complicated. If the provider did perform an excision, you won’t be able to report the excision and an I&D code per AHA HCPCS Coding Clinic (Volume 9, Issue 14), which tells you that “a physician excising pilonidal cysts and/or sinuses (CPT® codes 11770-11772) may incise and drain one or more of the cysts. It is inappropriate to report CPT® code 10080 or 10081 separately for the incision and drainage of the pilonidal cyst(s).” This guidance is reinforced by Correct Coding Initiative (CCI) edits that bundle I&D (10080 and 10081) into excision (11770-11772), with excision primary and I&D secondary.
But note this exception: If your clinician is performing I&D of a pilonidal cyst and, in another anatomic location, he excises another pilonidal cyst or sinus tract, then you can report both the procedures together. But, as CCI edits are in place, you will need to append either modifier 59 (Distinct procedural service) or possibly XS (Separate structure…) when billing Medicare or payers following Medicare rules to the 10080 or 10081, as this is the column 2 code in the edit list.
