Podiatry Coding & Billing Alert
Solve Non-Pressure Ulcers Conundrums by Checking Documentation for Healed Vs. Healing
If ulcer increases in severity during admission, report 2 codes. The ICD-10-CM Official Guidelines for Coding and Reporting offer so many helpful guidelines that can help you figure out how to appropriately report diagnosis codes on your claims. When it comes to chronic non-pressure ulcers, you have a lot of guidance to adhere to such as how to report healed non-pressure ulcers. Read on to learn more. Rely on These ICD-10-CM Codes for Chronic Non-Pressure Ulcers FAQ 1: Which ICD-10-CM codes do I have to pick from when coding chronic non-pressure ulcers of the foot, ankle, and toe? Answer: You should look to the following codes for non-pressure chronic ulcers of the foot, ankle, and toe: Handle Healed Non-Pressure Ulcers at Admission This Way FAQ 2: My podiatrist admitted a patient with a non-pressure chronic ulcer of the left heel and midfoot limited to breakdown of skin, but the ulcer healed at the time of admission. Can I report code L97.421 (Non-pressure chronic ulcer of left heel and midfoot limited to breakdown of skin) this case? Answer: No. You should not report a code if your podiatrist’s documentation states that the patient’s non-pressure ulcer was completely healed at the time of admission, according to the ICD-10-CM Official Guidelines for Coding and Reporting. Turn to These Codes for Healing Non-Pressure Ulcers FAQ 3: My podiatrist documented that an admitted patient has a non-pressure chronic ulcer that is healing. How should I report this on my claim? Answer: You could actually handle this in several different ways, all depending upon the information in the patient’s medical record. Scenario 1: If your podiatrist describes the non-pressure chronic ulcer as healing, you should report the correct non-pressure chronic ulcer code based upon the information in the documentation, per the ICD-guidelines. For example, you read in the medical documentation that the patient has a healing non-pressure ulcer of the right ankle limited to breakdown of skin. You would report L97.311 (Non-pressure chronic ulcer of right ankle limited to breakdown of skin) in this case. Scenario 2: If your podiatrist’s medical documentation does not provide information about the severity of the patient’s healing non-pressure chronic ulcer, you should instead report the appropriate code for unspecified severity. For example, you read in the medical documentation that the patient has a healing non-pressure chronic ulcer of the right ankle. However, this is all of the information your podiatrist provides. So, you would report L97.319 (Non-pressure chronic ulcer of right ankle with unspecified severity). Scenario 3: If your podiatrist’s documentation is not clear on whether the patient has a current (new) non-pressure chronic ulcer or whether your podiatrist is treating the patient for a healing non-pressure chronic ulcer, query your podiatrist for further clarification. Scenario 4: If the patient has an ulcer that was present at the time of admission but had healed by the time of discharge, you should report the appropriate ICD-10-CM code for the site and severity of the non-pressure ulcer at the time of admission. For example, you read in your podiatrist’s documentation that the patient was admitted with a non-pressure chronic ulcer of the left ankle with fat layer exposed, but the ulcer had healed by the time your podiatrist discharged the patient, you would report code L97.322 (Non-pressure chronic ulcer of left ankle with fat layer exposed). Report 2 Codes in This Instance FAQ 4: My podiatrist admitted a patient to an inpatient hospital with a non-pressure chronic ulcer of the right heel and midfoot limited to breakdown of skin. However, the ulcer progressed to a higher severity level during the patient’s admission. It moved to having the fat layer exposed. What code should I report? Answer: In this case, you should report two separate codes one code for the site and severity level of the ulcer on admission and a second code for the same ulcer site and the highest severity level reported during the patient’s stay. So, the first code you will report is L97.411 (Non-pressure chronic ulcer of right heel and midfoot limited to breakdown of skin). Then, you would report code L97.412 (Non-pressure chronic ulcer of right heel and midfoot with fat layer exposed) to represent the highest severity of the ulcer.

Related Articles
Podiatry Coding & Billing Alert
- CPT®:
Follow 5 Medicare Rules to Sidestep Common LOPS Errors for Diabetic Patient Claims
You must report an appropriate diabetes ICD-10-CM code on your claim. When your podiatrist sees [...] - FAQs:
Solve Non-Pressure Ulcers Conundrums by Checking Documentation for Healed Vs. Healing
If ulcer increases in severity during admission, report 2 codes. The ICD-10-CM Official Guidelines for [...] - X-rays:
Use Foot, Toe Modifiers to Secure Ethical X-Ray Reimbursement
Be aware of these NCCI edits before you report 73620 with 73660. A patient presents [...] - You Be the Coder:
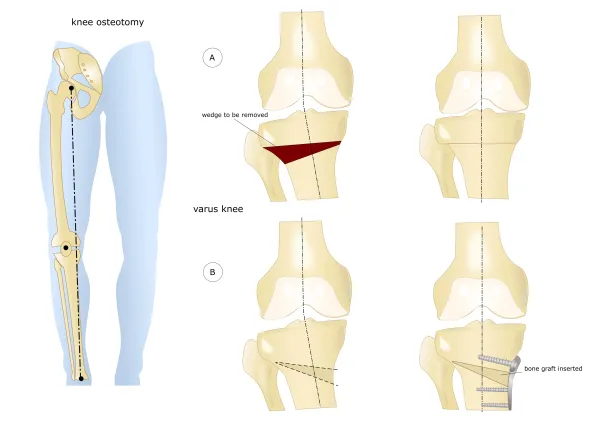
Distinguish Between Bimalleolar and Trimalleolar Fractures
Question: I’m new to coding, and I’m having trouble understanding the difference between different types [...] - Reader Questions:
Follow This Advice to Avoid Denials
Question: Medicare recently denied a claim citing invalid patient information. What could have caused this? [...] - Reader Questions:
Decipher Tumor Excision Code Choice
Question: My podiatrist excised a 2 cm in diameter tumor from just beneath the patient’s [...] - Reader Questions:
Focus on New MDM Guidelines
Question: If a provider is billing an outpatient E/M code based on medical decision making [...] - Reader Questions:
Find Exact Neuroplasty Code for 1 Nerve, 1 Toe
Question: My podiatrist used an open approach to incise scar tissue to relieve tension on [...] - Reader Questions:
Choose Appropriate Plantar Fascia Repair Code
Question: My podiatrist performed a fasciotomy of the patient’s foot and toe to relieve tension [...]