Podiatry Coding & Billing Alert
Diabetic Shoes:
Follow 3 Tips to Ace Diabetic Shoe Claims
Published on Thu Aug 18, 2022

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Podiatry Coding & Billing Alert
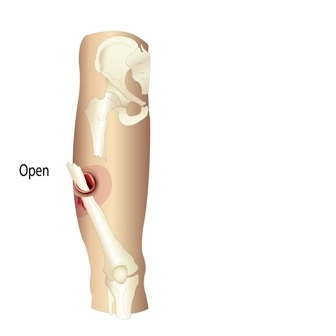
- Wound repair, Part 1:
Target Length of Wound and Complexity for Successful Laceration Repair
Wound repair using only adhesive strips should be reported with an E/M code. In the [...] - Diabetic Shoes:
Follow 3 Tips to Ace Diabetic Shoe Claims
Certifying physician must be MD or DO. When you bill for diabetic shoes in your [...] - E/M 2023:
Get Ready: Office/Outpatient Consultation CPT® Guidelines Will Change in 2023
Hint: Don’t forget to append modifier 32. Now is the time to review the changes [...] - You Be the Coder:
Puzzle Out This Arthrodesis Scenario
Question: The patient came in for right tarsometatarsal (TMT) joint fusion, which I thought would be [...] - Reader Questions:
See How to Submit Heel Spur Excision
Question: According to the documentation, my podiatrist performed a calcaneal spur resection with plantar fascial release [...] - Reader Questions:
Stay Compliant With HIPAA
Question: We’ve been experiencing an increase in phishing and are aware of reports of ransomware events. [...] - Reader Questions:
Understand Billing Date for Custom Inserts
Question: What would be the correct date of service to bill for custom inserts? The day [...]
View All