Podiatry Coding & Billing Alert
Case Study:
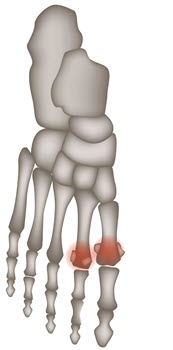
Solve This Compression Fracture Case in 3 Steps
Published on Wed Jan 17, 2024

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Podiatry Coding & Billing Alert
- Case Study:
Solve This Compression Fracture Case in 3 Steps
Be ready to consult three books to correctly code this scenario. In your podiatry practice, [...] - Quiz:
Resolve Ankle and Foot Effusion Coding Dilemmas by Answering These 8 Questions
Identifying the affected area is key to accurately coding this condition. In order to accurately [...] - Medicare Tips:
Avoid a Snag With These Medicare Signature Tips
Questionable signatures need resolution before claim submission. In your podiatry practice, you probably see Medicare [...] - You Be the Coder:
Sidestep Contusion Confusion With These Codes
Question: Our foot specialist recently examined a patient presenting with a bruise on their left foot. [...] - Reader Questions:
Amputation Location is Key to Coding Correctly
Question: I’m new to podiatry coding, and I’m trying to understand the difference between CPT® codes [...] - Reader Questions:
Protect Your Practice’s Digital Signatures
Question: In our recent risk evaluation, we discovered that the electronic signatures we and our patients [...] - Reader Questions:
Solve This Calcaneal Spur Conundrum
Question: The podiatrist carried out a removal of the calcaneal spur and released the plantar fascia [...]
View All