Pediatric Coding Alert
ICD-10:
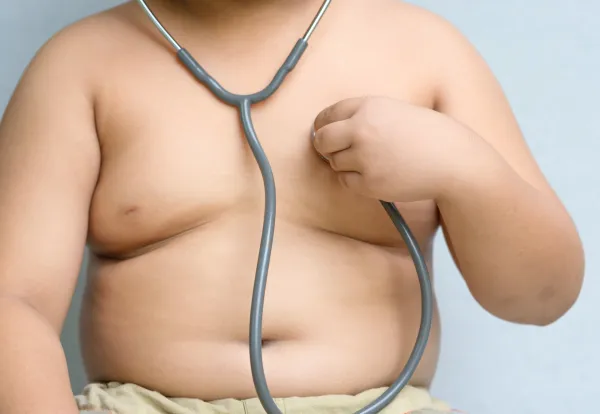
Confirm Obesity Specifics for Diagnosis Coding Options
Published on Wed Mar 30, 2016

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Pediatric Coding Alert
- 2016 News:
Consider These 3 CCI Manual Changes Before Coding Your Pediatric Services
The guidelines finally address how you should break down your time-based codes. The Correct Coding [...] - ICD-10:
Confirm Obesity Specifics for Diagnosis Coding Options
Yes, even pediatric patients can reach the ‘morbid’ category. In the not-too-distant past, some payers [...] - Medical Records:
Government Urges Practices to Stop Charging Patients for Medical Records
Although you can legally charge patients for sending their records, HHS appears to discourage it. [...] - How Much Can You Charge?
The Department of Health and Human Services technically allows practices to charge a fee to [...] - What If the Patient Disagrees With the Information in Her Records?
It happens from time to time—you share a copy of the patient’s medical records with [...] - Reader Question:
94664 Is Best Bet for Asthma Education
Question: We are starting to do asthma education with our asthma follow-up patients. Do I need [...] - Reader Question:
Look to 99188 for Fluoride
Question: Our pediatrician brushed fluoride onto a patient’s teeth. Can we report D1208 (Topical application of [...] - Reader Question:
Look to 99078 for Group Training
Question: Our physicians would like to perform group visits for about eight to ten patients at [...] - Reader Question:
Documentation Reigns for Cerumen Removal
Question: I enjoyed your article on the new cerumen removal code 69209 (Removal impacted cerumen using [...] - You Be the Coder:
Correction: Avoid 'X' Modifiers for E/M Codes
Question: In the Vol. 19, no. 4 issue of Pediatric Coding Alert, a reader asked whether [...]
View All