Pediatric Coding Alert
Make the Decision, Add Up the Points in This MDM Calculation
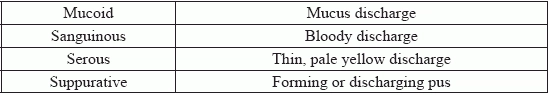
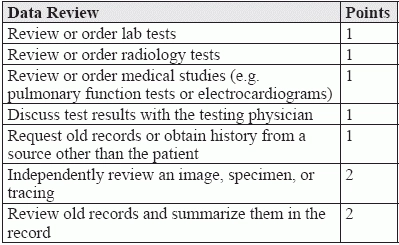
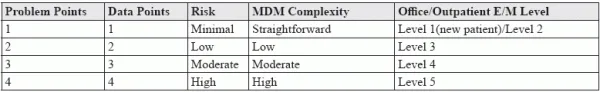
And know that numbers alone don’t always equate to the correct E/M level. More than history and the exam, the Centers for Medicare and Medicaid (CMS) regard medical decision making (MDM) “and time [as] the more significant factors in distinguishing visit levels” (Source: www.gpo.gov/fdsys/pkg/FR-2017-11-15/pdf/2017-23953.pdf). But calculating MDM often involves making judgement calls that can sometimes lead to upcoding or downcoding the evaluation and management (E/M) level for a particular encounter. That’s why, in order to make MDM calculations more objective, “CMS distributed a point system originally developed by the Marshfield Clinic to Medicare carriers to be used on a voluntary basis,” according to Mary I. Falbo, MBA, CPC, CEO of Millennium Healthcare Consulting Inc. in Lansdale, Pennsylvania. Whether or not you use the point system to determine the complexity of MDM in an E/M level calculation, it is important for you to understand how it works. That’s because “Medicare contractors use the system to audit MDM,” Falbo points out. So, too, do payers that follow Medicare guidelines. So, we’ve put together this scenario to see how you would score the MDM involved and arrive at the appropriate E/M level. The Scenario Your pediatrician sees a female patient for a follow-up after the patient was previously diagnosed with her fourth case of otitis media in six months. The patient still complains of ear pain after finishing her antibiotics. The patient also complains of a sore throat that is so painful that she sometimes has difficulty swallowing. The pediatrician takes the patient’s medical history from her mother, and orders a strep test for the sore throat, which comes back positive. The provider diagnoses strep pharyngitis and prescribes another antibiotic. Score the Dx and Treatment Options The first points you calculate will be based on the following table Based on the scenario, you would assign three problem points for the new problem without a planned workup, as the workup has already been completed. Score the Data Points Next, you’ll calculate the points for the review of the patient’s medical history and the lab order using this table: For ordering the rapid strep test and taking the history from a source other than the patient, you’ll score two points. Calculate the Level of Risk The last component of MDM, the level of risk, is the only one not scored. To determine risk, you’ll need to consult a chart such as the one CMS provides at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/eval-mgmt-serv-guide-ICN006764.pdf). In this case, you have a chronic illness with a mild exacerbation, leading you to score a moderate level of risk based on the chronic otitis and the acute strep pharyngitis. Coding caution: As easy as all this sounds, “determining risk level is where the gray areas come in, as there are several items that can impact your decision,” warns Chelle Johnson, CPMA, CPC, CPCO, CPPM, CEMC, AAPC Fellow, billing/credentialing/auditing/coding coordinator at County of Stanislaus Health Services Agency in Modesto, California. “Items such as the number of conditions, whether they are acute or chronic, whether the drugs are prescription or over the counter, and so on can all change the leveling of MDM,” Johnson continues. Putting it all Together You’ll use the following chart to determine the MDM level: Under the scoring system, you have three problem points for the diagnosis, two data points and a moderate level of risk. As levels for two of the three components must be met or exceeded to assign MDM complexity, this would lead you to assign a moderate MDM complexity level to this encounter. But that, in and of itself, does not mean you can leap to assign a level-four E/M code to the visit. That’s because “even though you may use the point system to justify the E/M level your provider has performed, the most important factor in determining the appropriate level is medical necessity,” Falbo cautions. “Even if there is a large amount of documentation to justify the choice, the E/M level must match the patient’s condition and the treatment options that it necessitates,” Falbo concludes. In other words, no matter what the MDM complexity level, the chief complaint and presenting problems should determine the type of history obtained as well as the type of exam that is medically necessary to treat the patient for the presenting problems. The Final Word Whether you use the system to code encounters like this or not, it is important to be aware that the system is not perfect. “The system still leaves a lot of areas that can become battlegrounds during audits,” Johnson warns. This means your office should have clear policies in place regarding those gray areas, especially when determining the level of risk. “That way, if you are audited, you will be able to show consistency in your determinations,” Johnson argues.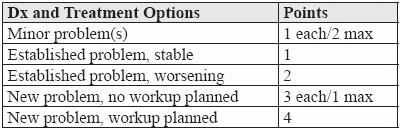
Related Articles
Pediatric Coding Alert
- Practice Management:
Take These 4 Steps to Perform Successful, Stress-Free Self-Audits: Part 1
Our experts offer insights, proven strategies for this important management tool. Self-audits are a little [...] - Guidelines:
Make the Decision, Add Up the Points in This MDM Calculation
And know that numbers alone don’t always equate to the correct E/M level. More than [...] - Clip & Save:
Use This Chart for Accurate ADHD/ADD/Coexistent Condition Coding
Don’t let subtle differences between conditions lead to coding errors. On the surface, diagnosis coding [...] - You Be the Coder:
Follow This Advice, Calculate Risk Level With Confidence
Question: I’m trying to determine the level of risk in the following encounter: a patient [...] - Reader Question:
Keep Areas, Systems Separate for Accurate E/M Levels
Question: We are performing a voluntary self-audit of our evaluation and management (E/M) codes. As [...] - Reader Question:
Test Your Understanding of This Inclusive Dx
Question: We just got denied on a claim billed for strep and influenza A and [...]