Prep Now for New Consultation, Speech Evaluation Codes
CPT® 2014 also offers several new vaccine codes.
Just like an early holiday present, CPT® delivers the goods this year with news that several new, revised and deleted codes will be waiting for you effective Jan. 1. Although we gave you a sneak peek at these coding changes in last month’s issue of Pediatric Coding Alert, we’ve got more in-depth insight this month. Read on to find out what you’ll be facing when the calendar turns to 2014.
Consultations Are Not Just a Thing of the Past
Effective Jan. 1, CPT® will include four new codes that describe the work of two medical professionals who discuss a patient’s condition via phone or internet, as follows:
“The interprofessional codes are interesting,” says Suzan Berman, MPM, CPC, CEMC, CEDC, manager of physician compliance auditing for West Penn Allegheny Health Systems, Pittsburgh, Penn. “More and more, the provider community is communicating with patients via the internet through secure email lines, etc. A lot of health plans and insurance carriers are offering their members access to health records and their healthcare providers or case representatives on-line. These avenues give patients the ability to check their records, confirm what their doctors told them, ask further questions, question potential mis-recorded information, etc. These codes appear to be in recognition of these situations. It affords the physician the ability to forward patient information (securely) to another physician for opinion and insight without having the patient come to all the different appointments.”
As in the past, these new codes are consultative in nature, which means you must provide a written report back to the requesting physician to qualify for the code, as indicated by the phrase “including a verbal and written report” (emphasis added).
More questions: Coders and consultants alike have many questions about these new codes. “I am a bit curious about why they are broken into time and how that time will be measured (reading, discussing, interpreting, further research, etc.).
How will the time be documented?” Berman asks. “Will it be documented? What will the reimbursement look like in comparison with having the patient actually come into the office?”
“The physicians will want to know if it is something they might be able to utilize,” says Chandra L. Hines, practice supervisor of Wake Specialty Physicians in Raleigh, NC, who echoes many coders interested in determining whether insurers will include payment for these codes, since they are consultations. Keep an eye on Pediatric Coding Alert for more on whether these are payable once the 2014 insurance fee schedules are released.
99481/99482 Replace Category III Codes
You’ll find two new neonate hypothermia codes among the E/M code changes as well. CPT® 2014 adds the following:
“These are highly specialized neonatal codes and are not used by most pediatricians,” says Richard Tuck, MD, FAAP, pediatrician at PrimeCare of Southeastern Ohio in Zanesville.
These new codes seem to replace Category III codes 0260T (Total body systemic hypothermia, per day, in the neonate 28 days of age or younger) and 0261T (Selective head hypothermia, per day, in the neonate 28 days of age or younger), which will be deleted in 2014.
Reminder: When a category III code exists to describe a service or procedure, you must use that category III code — rather than an unlisted procedure code — to describe the service when placing a claim. So, why is this so important?
Category III CPT® codes are temporary codes that describe emerging technology, services, and procedures.
The primary purpose of these codes is to allow for data collection, which in turn provides information for evaluating the effectiveness of new technologies and the formation of public and private policy. In other words, category III codes give insurers and government policy makers a way to track the effectiveness and rate-of-use of as yet unproven technologies, which could affect future coverage decisions.
New Vaccine Codes Help With Flu Shot Coding
Last year, the CPT® Editorial panel announced four influenza vaccine codes that went into effect in January, but they weren’t printed in the CPT® book. However, your 2014 manual will include the codes, as follows:
These codes are essentially the quadrivalent version of codes 90655-90658, and most practices are looking forward to administering them. Keep in mind, however, that there will be supply and payment issues related to these new vaccines and it’s unclear whether insurers will recognize them, and whether they will pay enough to cover the cost given that the quadrivalent vaccine will cost your practice more money. Medicare recently assigned the prices of $23.228 to 90685 and $19.409 to 90686, but payment amounts for 90687 and 90688 are still pending. Although pediatric practices don’t typically bill Medicare, many private payers do follow the agency’s lead on setting prices.
Caveat: Both 90687 and 90688 carry the lightning bolt symbol in AMA materials indicating that FDA approval is pending. So check for FDA approval of each vaccine represented by the code before using the associated code.
In addition, CPT® 2014 will introduce new code 90673 (Influenza virus vaccine, trivalent, derived from recombinant DNA (RIV3), hemagglutinin (HA) protein only, preservative and antibiotic free, for intramuscular use), which was released on July 1 of this year.
Speech Evaluation Gets Specific
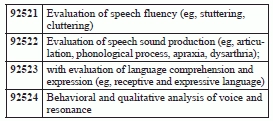
CPT® will also eliminate the vague code 92506 (Evaluation of speech, language, voice, communication, and/or auditory processing) that you’ve been using to evaluate patients’ speech issues. Instead, 2014 will bring heightened specificity to these options, with the following new codes:
Going forward, you will be able to more clearly differentiate between your evaluations of stuttering (92521) and evaluations of apraxia (92522) thanks to the new codes.
Keep in mind: Until the annual publication of the CPT® code set, small further revisions may occur to the 2014 codes. Keep an eye on Pediatric Coding Alert for additional news on the new codes.