Pediatric Coding Alert
Weigh the Answers to These Frequently Asked Pediatric BMI Questions
And take heed of these 3 notes of caution. Coding for a pediatric patient’s body mass index (BMI) isn’t as simple as it looks. Unlike adult BMIs, children’s BMIs are calculated as percentiles relative to their gender and age group. And even when you locate the correct code, knowing when you can, or should, use it can also be pretty tricky. So, we answered six of the most frequent questions about pediatric BMI coding, and added some notes of caution, to help you get everything straight. What Is BMI? According to the Centers for Disease Control and Prevention (CDC), BMI “is a person’s weight in kilograms divided by the square of height in meters.” So, a 7-year-old boy who is 121.9 cm and weights 22.9 kg would have a BMI of 15.4. Not good at math? Don’t worry. “An easy way to calculate this is to go to the BMI calculator available on the CDC website,” says Chelle Johnson, CPMA, CPC, CPCO, CPPM, CEMC, AAPC Fellow, billing/credentialing/auditing/coding coordinator at County of Stanislaus Health Services Agency in Modesto, California. Simply plug a patient’s height and weight information into the calculator, which you can find at www.cdc.gov/healthyweight/bmi/calculator.html, and let it do the rest. Coding caution 1: “Many electronic medical records [EMRs] will now provide the calculation as well, though if only the patient’s height and weight are documented, I would not recommend assigning a BMI code since the BMI was not documented,” notes JoAnne M. Wolf, RHIT, CPC, CEMC, coding manager at Children’s Health Network in Minneapolis. Why Is BMI Important? As “a high BMI can be an indicator of high body fatness,” a patient’s BMI “can be used to screen for weight categories that may lead to health problems,” though “it is not diagnostic of the body fatness or health of an individual,” according to the CDC. This means a child’s BMI does not tell the full story of that child’s health, but it can be a significant indicator or predictor of possible problems. Why Do Adult and Pediatric BMI Calculations Differ? As children’s heights and weights change rapidly as they develop, so too does their body fat. Accordingly, a child’s BMI will fluctuate more than an adult’s, so it is “interpreted relative to other children of the same sex and age” and “expressed as a percentile,” the CDC explains. This means a child’s BMI must then be plotted on a chart such as the ones the CDC provides: BMI-for-age percentiles for boys: www.cdc.gov/growthcharts/data/set1clinical/cj41l023.pdf. BMI-for-age percentiles for girls: www.cdc.gov/growthcharts/data/set1clinical/cj41l024.pdf. How Does This Relate to Coding? If the patient’s BMI is documented in the medical record, you should assign the specific code from the following: Who Can Document BMI? ICD-10 guideline 1.B.14 determines who can document a code from Z68.-. Unlike most code assignments, which must be “based on the documentation by [the] patient’s provider,” the guideline goes on to state that BMI may be assigned based “on medical documentation from clinicians who are not the patient’s provider … since this information is typically documented by other clinicians involved in the care of the patient (e.g. a dietitian often documents the BMI …).” Coding caution 2: However, the guideline goes on to say that “the associated diagnosis (such as overweight [or] obesity …) must be documented by the patient’s provider.” So, “if there is conflicting medical documentation … the patient’s attending provider should be queried for clarification.” When Should You Use a BMI Code? Guideline 1.C.21.c.3 states that the “BMI codes should only be assigned when there is an associated reportable diagnosis (such as obesity)” (emphasis retained). This corresponds to the instructions for ICD-10 codes R63.6 (Underweight) and E66.- (Overweight and obesity), which tell you to “use [an] additional code to identify body mass index (BMI) if known.” It also follows ICD-10 guideline 1.B.14, which reminds you that “BMI … should only be reported as secondary diagnoses.” Coding caution 3: “If a pediatrician documents ‘overweight,’ it is simple enough to code E66.3 [Overweight]. But you should not add an obesity or overweight diagnosis code just from a BMI calculation,” cautions Wolf. Instead, “you should only code a diagnosis that the provider has actually documented in the medical record,” Wolf recommends. That’s because “there may be times that a patient has a high BMI but is not considered overweight or obese, as is the case with some athletes due to muscularity,” notes Johnson. Consequently, you should read the assessment provided by your pediatrician before assigning the code.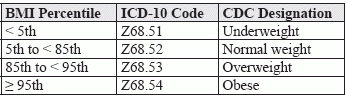
Related Articles
Pediatric Coding Alert
- News You Can Use:
Note These Extensive NCCI Edits for Online Digital E/Ms
Make sure you bill email communications correctly this year. Late last year, the Centers for [...] - Mythbusters:
Bust These 4 Myths, Preclude Preventive Service Claim Errors
Knowing what is, what is not, included is key. Preventive services are the lifeblood of [...] - Condition Spotlight:
Weigh the Answers to These Frequently Asked Pediatric BMI Questions
And take heed of these 3 notes of caution. Coding for a pediatric patient’s body [...] - You Be the Coder:
Don't Prolong This Neonatal Intensive Care Service
Question: If we bill 99468 for neonatal intensive care, can we also bill a prolonged [...] - Reader Question:
Examine This Encounter, Claim This Code
Question: Our pediatrician just saw a 4-year-old patient for a new patient well-child check. Due [...] - Reader Question:
Know When, When Not, to Report Professional Service Component
Question: I’m hoping you can provide clarification on the appropriate date of service (DOS) when [...] - Reader Question:
Choose This Code for Higher Level of Neonate Care
Question: Our pediatrician was making rounds at the local hospital and transferred a newborn patient [...]



.webp)
