Pediatric Coding Alert
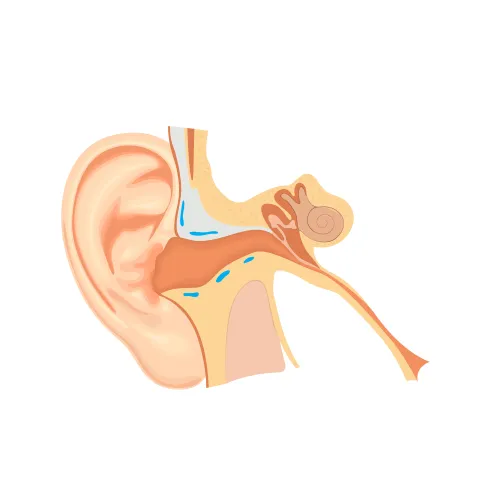
Cerumen Removal:
This Payer Outlines How to Collect for New Cerumen Removal Code 69209
Published on Wed Feb 17, 2016

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Pediatric Coding Alert
- Cerumen Removal:
This Payer Outlines How to Collect for New Cerumen Removal Code 69209
Plus: CCI weighs in on the issue. It’s been active for over a month now, [...] - ICD-10:
Random-Order Diagnoses Could Cost You
Implement this ICD-10 action plan to decide which diagnosis should go first. In situations when [...] - Electronic Health Records:
Follow 3 Quick Steps to Calm Down If Your EHR Acts Up
No one wants an EHR to go offline, but you can avoid panic with these [...] - You Be the Coder:
Can You Define 'Normal?'
Question: We almost always report normal newborn care codes for the pediatrician’s visits to the hospital [...] - Reader Question:
Cheat Sheets Are Just a Starting Point
Question: We have been training our new pediatricians to use the superbills we printed with our [...] - Reader Question:
Discharge Code Limited to One Provider
Question: One of our patients had a complex health history and we were among four different [...] - Reader Question:
Consult Guidelines for Tricare Coverage
Question: I remember hearing that Tricare covers speech therapy but we keep getting denials for it, [...] - Reader Question:
Correct EHR Entries As You Would Paper
Question: We are aware of how to correct a mistake on a paper medical record, [...]
View All