Pathology/Lab Coding Alert
Get the Answers to Your Frequently Asked Genetic Testing Questions
Here’s how to make your way through the CPT® molecular pathology code set.
“The genetic testing code set is really unlike anything else in CPT®,” explained Larry Simon, MD, MBA, Blue Cross and Blue Shield of Louisiana, Member CPT® Editorial Panel, in his presentation More Than Denim - Understanding Genes, Biomarkers, and Molecular Pathology with Aaron D. Bossler, MD, PhD, Moffitt Cancer Center, Tampa, Member CPT® Editorial Panel at HEALTHCON 2024.
So if you’re bewildered by the ever-growing number of molecular pathology tests available to analyze a patient’s genetic makeup, and you couldn’t make it to the session, you’ve come to the right place.
Here’s some of what you missed.
What Is Genetic Testing?
Essentially, our bodies’ DNA or RNA, “encodes all the proteins that make up our cells that make up our tissues that make up our bodies that make us, ‘us’,” Bossler explained. DNA or RNA — also known as biomarkers, molecular markers, or signature molecules — are subject to different types of mutations: one nucleotide in a sequence can change to another, for example, or a DNA sequence can be deleted or inserted in both small and large ways. All of these things can affect a patient’s propensity to a given disease as well as their ability to be able to fight it.

Genetic testing, then, enables providers to do a number of things for their patients: providers can use the tests to confirm a diagnosis; predict how a patient’s genetics will affect their response to treatments; counsel a patient on the genetic etiology of a disease so they can make decisions about treatments or disease management; and predict the progression of a disease.
For example, a deletion in the EGFR gene removes some key amino acids, a mutation that makes lung cancer patients sensitive to tyrosine kinase inhibitors. Somatic testing — testing that looks for acquired mutations in an individual and is used to detect such conditions as cancer or neoplasia — allows such patients to see if they will, or will not, respond to tyrosine kinase inhibitors, a targeted cancer therapy that attacks certain cancer cells while leaving other cells alone, Bossler explained.
How Are the Genetic Testing Codes Structured in CPT®?
“There are codes for essentially single genes, then codes for a bunch of genes tested at one time, codes for a bunch of genes tested at one time plus a bunch of other stuff thrown in like a gumbo, then a separate set of codes that are for your lab, and no one else can use them but you,” explained Simon.
Tier 1 Codes (81161-81399) are specific to single genes. For example, 81205 (BCKDHB (branched-chain keto acid dehydrogenase E1, beta polypeptide) (eg, maple syrup urine disease) gene analysis, common variants (eg, R183P, G278S, E422X)) tests for mutations in the BCKDHB gene, which can “disrupt the normal function of the BCKD enzyme complex, preventing it from effectively breaking down leucine, isoleucine, and valine … leading to seizures, developmental delay, and the other health problems associated with maple syrup urine disease,” according to Medline Plus (https://medlineplus.gov/genetics/gene/bckdhb/#conditions).
These tests must “demonstrate clinical usefulness,” and must have widespread and high volume of utilization in labs across the U.S., according to Simon.
Tier 2 Codes (814400-81408, 81479) cover a wide range of genes. For example, 81400 (Molecular pathology procedure, Level 1 (eg, identification of single germline variant [eg, SNP] by techniques such as restriction enzyme digestion or melt curve analysis) …) lists 23 different genes that can be tested using this methodology. However, these tests are usually performed at a much lower volume than the Tier 1 tests.
Essentially, the two tiers reflect the resources involved in performing and interpreting the tests.
Multianalyte Assays with Algorithmic Analyses (MAAA) Codes (81490-81599) and Administrative MAAA Codes (0002M-0019M) describe procedures that use multiple results and an algorithmic analysis from the testing of genes, proteins, lipids, and carbohydrates, and are usually unique to a single laboratory or manufacturer, Simon explained. Administrative MAAA codes are similar to Category III CPT® codes, in that the tests have lower utilization and literature support than Category I codes.
Examples include 81521 (Oncology (breast), mRNA, microarray gene expression profiling of 70 content genes and 465 housekeeping genes, utilizing fresh frozen or formalin-fixed paraffin-embedded tissue, algorithm reported as index related to risk of distant metastasis), which is unique to MammaPrint®, Agendia, Inc., and 0006M (Oncology (hepatic), mRNA expression levels of 161 genes, utilizing fresh hepatocellular carcinoma tumor tissue, with alpha-fetoprotein level, algorithm reported as a risk classifier), which is unique to HeproDXTM, GoPath Laboratories, LLC.
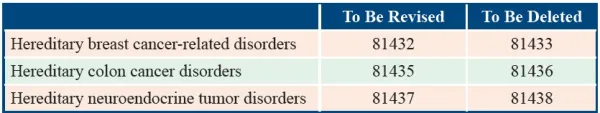
Genomic Sequencing Procedure Codes (81410-81471) are performed on nucleic acids from germline or neoplastic samples to analyze DNA or RNA sequencing “relevant to a clinical situation,” according to Simon. An example of these codes would be 81435 (Hereditary colon cancer disorders (eg, Lynch syndrome, PTEN hamartoma syndrome, Cowden syndrome, familial adenomatosis polyposis); genomic sequence analysis panel, must include sequencing of at least 10 genes, including APC, BMPR1A, CDH1, MLH1, MSH2, MSH6, MUTYH, PTEN, SMAD4, and STK11).
Proprietary Laboratory Assays (PLA) Codes (0001U-0999U) describe codes that are unique to a lab or manufacturer that wants to specifically identify their test, and must be used over a Category I code for the same service because the PLA code is more specific, Simon notes.
An example of a PLA code is +0162U (Hereditary colon cancer (Lynch syndrome), targeted mRNA sequence analysis panel (MLH1, MSH2, MSH6, PMS2) (List separately in addition to code for primary procedure), a test proprietary to CustomNext + RNA: Lynch (MLH1, MSH2, MSH6, PMS2), Ambry Genetics®.

Reminder: All the genetic testing codes must fulfill the CPT® criteria for Category I codes, meaning the service must:
- Be cleared or approved by the FDA when required for performance of the service;
- Be “performed by many physicians or other qualified health care professionals across the United States”;
- Be “performed with frequency consistent with the intended clinical use (ie, a service for a common condition should have high volume …”);
- Be “consistent with current medical practice”; and
- Be “documented in literature” for its “clinical efficacy” meeting the requirements “set forth in the CPT® code change application” per CPT® guidelines.
When Does CPT® Update the Molecular Pathology Codes?
“The lab CPT® code set is changed multiple times a year. It’s really important to keep up with this release calendar in order to configure your systems and code for things properly,” cautioned Simon.
This means paying attention to more than just the annual CPT® updates that are released at the end of September every year and that become effective on Jan. 1 of the following year. That’s because these updates only affect the Tier 1 molecular pathology test codes. The AMA updates the PLA codes on a quarterly basis, however, while the Tier 2 and MAAA codes are updated three times a year per the schedule found in the Code Changes Beyond the Annual Code Set Release Cycle chart located on page 1330 of the 2024 CPT® book.
Related Articles
Pathology/Lab Coding Alert
- Molecular Pathology:
Get the Answers to Your Frequently Asked Genetic Testing Questions
Here’s how to make your way through the CPT® molecular pathology code set. “The genetic [...] - Billing:
Address These Key Fields, Complete ABNs With Ease
Don’t forget that every ABN form must be one single page. As every pathology practice [...] - Compliance:
Stay on the Right Side of the Stark Law With Key Strategies
Scrutinize your referrals to avoid inadvertent violations. Every lab has seen news headlines trumpeting multimillion [...] - You Be the Coder:
Be Wise to Zika Virus Coding
Question: Our lab performed a blood test for Zika virus antigen detection for a patient presenting [...] - Reader Questions:
Rely on These Tips for Bone Cases
Question: During hip replacement surgery for a patient with severe osteoporosis, the surgeon submits the [...] - Reader Questions:
Focus Blood Type Reporting
Question: We received a paternal blood specimen for blood typing as part of the neonatal care [...]