Pathology/Lab Coding Alert
Fortify Diagnosis Coding With 3 Q/A Scenarios
Grasp your lab’s contribution to final Dx.
Whether your clinical lab receives a narrative diagnosis for a test order, or your pathologist makes a final diagnosis from a specimen exam, lab coders need to comprehend ICD-10-CM usage in many different situations.
With the following questions and our experts’ answers, you can discover when and how your lab’s work impacts or dictates final diagnosis coding.
Pathology Assigns Final Dx
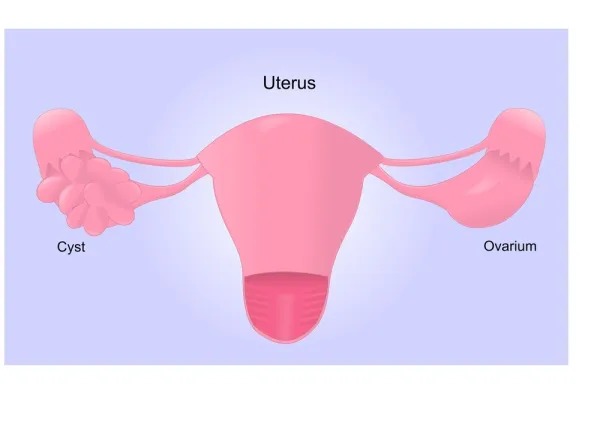
Question 1: The pathologist examines a breast biopsy of a right breast mass for a patient with a history of carcinoma in situ of ovary and cervix. The pathology report’s microscopic section describes “myoepithelial cells present in parallel arrangement,” and the diagnosis section states, “intraductal hyperplasia.” What diagnosis code(s) should we report?
Answer 1: Because the pathology report provides a final diagnosis, that’s what you should list as the primary diagnosis code. The correct code for intraductal hyperplasia of right breast is N60.81 (Other benign mammary dysplasias of right breast).
Because the clinician provided information about the history of in situ cervical and breast cancer, you may list a secondary diagnosis of (Z86.000, Personal history of in-situ neoplasm of breast) and (Z86.001, Personal history of in-situ neoplasm of cervix uteri).
Avoid: Don’t code a primary malignancy that has previously been excised and is no longer the subject of treatment, according ICD-10-CM coding guidelines. That means you shouldn’t report the past breast or uterine neoplasms using codes such as D05- (Carcinoma in situ of breast) and D06- (Carcinoma in situ of cervix uteri).
Symptoms May Lead Dx Choice
Question 2: An Ob/Gyn submits an incidental vaginal mucosa specimen from a patient during an endometrial ablation procedure. The clinician indicates the patient has undergone past endometrial ablations and suffers cyclic pelvic pain and hematometra. The pathologist confirms normal vaginal mucosa. What diagnosis and procedure codes should you use?
Answer 2: The correct procedure code is 88302 (Level II - Surgical pathology, gross and microscopic examination … vaginal mucosa, incidental …). Because the pathologist doesn’t provide a diagnosis beyond confirmation of normal vaginal mucosa , you’ll need to use the clinician’s ordering diagnosis for this case.
If the op note doesn’t provide an ICD-10-M code, you may assign a code based on the narrative diagnosis, such as cyclic pelvic pain (R10.2, Pelvic and perineal pain) and hematometra (N85.7, Hematometra), and history of endometriosis (Z87.42, Personal history of other diseases of the female genital tract).
New: This case may be a patient with post endometrial ablation syndrome, which typically includes symptoms such as cyclic pelvic pain and retention of blood in the uterus (hematometra). You should be aware of the following upcoming diagnosis code that reflects the condition, says Melanie Witt, RN, MA, an independent coding consultant in Guadalupita, New Mexico: N99.85 (Post endometrial ablation syndrome). You may want to consult the clinician who sent the specimen to determine if N99.85 (effective Oct. 1, 2019) or symptom codes, such as those previously mentioned, are the most appropriate for this case.
Duck the Pathogen Problem
Question 3: The clinician sends two urine specimen tubes for complete urinalysis with reflex to culture. That means the lab will automatically culture the second tube to identify microorganisms if findings from the initial urinalysis indicate a possible urinary tract infection.
The lab performs an automated complete urinalysis and reflexes to urine culture based on initial findings of elevated white blood cells (WBC) in the urine. The culture performed on the second specimen does not isolate and identify any organisms. What are appropriate codes for this scenario?
Answer 3: Report the urinalysis as 81001 (Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrite, pH, protein, specific gravity, urobilinogen, any number of these constituents; automated, with microscopy), and the urine culture as 87086 (Culture, bacterial; quantitative colony count, urine).
Findings: “It’s not unusual for a urine specimen to be virtually sterile and not show significant colony growth,” says William Dettwyler, MT AMT, president of Codus Medicus, a laboratory coding consulting firm in Salem, Ore. The only finding from this scenario is pyuria, which is WBC in the urine.
Diagnosis coding problem: If you look up “pyuria” in the ICD-10-CM index to find the appropriate code, you’ll be directed to the code for a urinary tract infection (UTI): N39.0 (Urinary tract infection, site not specified). Turning to that code, you’ll see an instruction to “Use additional code (B95-B97), to identify infectious agent.” But in this case, you have no infectious agent, and no real reason to diagnose the patient with a UTI. In fact, WBC in urine could indicate other conditions besides UTI, such as inflammation, kidney stone, or tumor.
Diagnosis Solution: As of Oct. 1, 2019, you have a new code for pyuria that would accurately reflect the findings in this case, instead of erroneously attributing the findings to an infection. The new code is R82.81 (Pyuria).
Alert: Although clinical labs typically provide the test results to the clinician without assigning a final diagnosis, you should be aware of the new R82.81 code, because it may become a key to indicate medical necessity for the reflex culture test.
Related Articles
Pathology/Lab Coding Alert
- Clinical Lab:
Master PSA Test Claims in 4 Steps
Grasp code and compliance tips. If your lab runs plenty of prostate specific antigen (PSA) [...] - ICD-10-CM:
Fortify Diagnosis Coding With 3 Q/A Scenarios
Grasp your lab’s contribution to final Dx. Whether your clinical lab receives a narrative diagnosis [...] - Medicare:
You're Not Immune to Fraud and Abuse Charges
Some coding practices could trap you. If you’re holier-than-thou about healthcare providers who are accused [...] - You Be the Coder:
Capture Each Bone Marrow Biopsy Step
Question: Our pathologist examined an iliac crest bone marrow biopsy following decalcification. The case involved [...] - Reader Question:
Take These Tick-Bite Tips
Question: When a patient has a tick bite and the clinician orders a test for [...] - Reader Question:
Distinguish Clinical Panel Test from Panel Code
Question: Our lab performs the obstetrics panel, but we use the automated treponemal antibody test [...]