ICD-10 Glitch Sinks Some Foot Care Claims

Plus: Yes you can translate your own handwriting for MAC review.
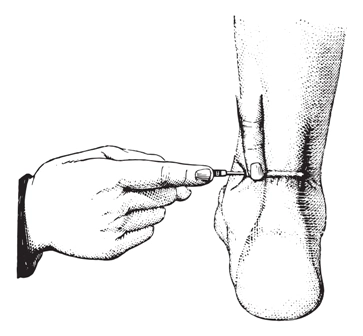
Although most ICD-10 claims are flowing smoothly, practices are still facing glitches following the rollout of the new diagnosis coding system, which went into effect just over two months ago. The latest victims? Routine foot care and nail debridement claims, which are being denied inappropriately, one MAC recently announced.
“Some claims for routine foot care and debridement of nails have processed incorrectly since the transition to ICD-10,” said NGS Medicare in a Dec. 2 news blast. “NGS is adding some diagnoses as payable for these services and correcting edits which resulted in incorrect denials.”
While that’s good news for practices that were reporting payable services, NGS also had some bad news for practices whose claims didn’t meet Medicare payment criteria. “NGS has also identified submitted claims were paid for some services which did not meet overage criteria have been allowed in error.”
Therefore, whether your foot care claims were denied or paid inappropriately, the MAC is performing a mass adjustment to either pay or recoup reimbursement, so you don’t have to do anything to get the corrections made.
In other news…
When Medicare payers come calling for your documentation to support claims, you may be faced with a dilemma—submit illegible records that the MAC may not be able to read, or send nothing and expect to have to pay back all the money you collected for the services. Fortunately, one Part B MAC has a third option.
“If a provider feels that his/her notes may not be legible, he/she may translate these notes prior to submitting them to Palmetto GBA for review,” the MAC said in a Nov. 25 tip on its website. “The note must be translated verbatim and signed by the provider.” You must then submit both sets of notes—the illegible and the translated version—to the payer for review.