Check out four scenarios that highlight the coding nuances.
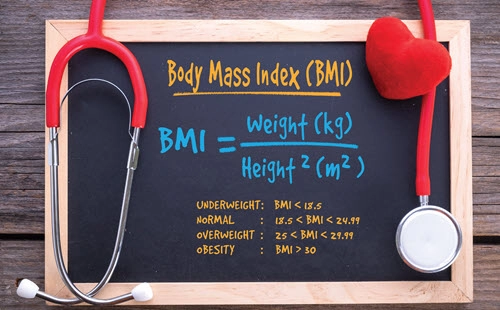
When you enter a patient’s height and weight into a body mass index (BMI) calculator, and the result falls within the 25.0–29.9 range — the person is considered overweight, according to the Centers for Disease Control and Prevention (CDC) guidance.
If that number is 30 or above, then the CDC regards the person as obese. However, there are different factors that complicate the process of assigning a BMI, overweight, or obesity diagnoses — and related codes. Read on for four scenarios that help you know when you should, and should not, use the codes.

Know When You Cannot Code BMI or Overweight/Obesity
Scenario 1: During a preventive physical exam, your provider documents that a patient is 5 feet 3 inches tall and weighs 225 pounds. The provider documents in the note that he has counseled the patient about the need to lose weight and the importance of exercise and good nutrition.
In this scenario, even though it is possible to calculate that the patient’s BMI is 39.9 — well in the range of what the CDC designates as obese — you cannot report a code from E66.- (Overweight and obesity) based on BMI. That’s because the provider has not documented a primary diagnosis of obesity in the scenario.
In fact, you should never assume a relationship between a patient’s BMI and a weight-related condition. While the two are often linked, they do not always correlate. For example, “there may be times that a patient has a high BMI but is not considered overweight or obese, as is the case with some athletes due to muscularity,” notes Chelle Johnson, CPMA, CPC, CPCO, CPPM, CEMC, AAPC Fellow, billing/ credentialing/auditing/coding coordinator at County of Stanislaus Health Services Agency in Modesto, California.
Additionally, even though you can calculate a BMI of 39.9 based on the patient’s height and weight, you cannot document that either. “If only the height and weight were documented, I would not recommend assigning a BMI Z code since the BMI was not documented,” says JoAnne M. Wolf, RHIT, CPC, CEMC, coding manager at Children’s Health Network in Minneapolis.
What you should code: In this case, you can really only code Z00.00 (Encounter for general adult medical examination without abnormal findings), assuming the exam was the only purpose for the patient’s visit and your clinician provided no other services during the encounter.
Know When You Cannot Code BMI
Scenario 2: A patient reports to your provider with severe pain in the right ear. Your provider takes the patient’s vitals and notes a BMI of 28.9 along with a diagnosis of acute serous otitis media, right ear (H65.01).
In this encounter, you cannot code for the BMI as the diagnosis your provider has reported is not weight related. A patient’s BMI is only relevant in cases where a provider has recorded conditions such as malnutrition, eating disorders, under- or overweight, or obesity. Only then should you use a BMI code. This is consistent with ICD-10 guidelines that BMI “should only be reported as secondary diagnoses” and “when there is an associated, reportable diagnosis (such as obesity)” (emphasis added).
What you should code: Only H65.01 should be entered into the medical record for this encounter.
Know When You Can Code Overweight/Obesity but not BMI
Scenario 3: Your provider records a diagnosis of overweight in the patient’s record. The provider has documented the patient’s height (6 feet) and weight (200 pounds) in the medical record, but not the patient’s BMI.
In this case, even though the patient’s BMI, which calculates to 27.1, and the overweight diagnosis are linked, you still cannot code the BMI as, similar to the first scenario, the provider has not entered the BMI into the record.
What you should code: In this scenario, even though you cannot report the patient’s BMI, you can report E66.3 (Overweight) due to the provider’s documentation.
Know When You Can Code BMI, but not Overweight/Obesity
Scenario 4: Your provider documents a patient’s weight and height. Based on the statistics, the provider records a BMI of 32.5.
Per the CDC tables, this patient’s weight status is obese. However, as the provider has not recorded that diagnosis, neither can you.
Simply put, “if a clinician documents ‘obese,’ it is simple enough to pick a code from E66.-. But I do not recommend adding an obesity or overweight diagnosis code just from a BMI calculation; instead, you should code a diagnosis that the provider actually documented in the medical record,” argues Wolf.
What you should code: In this scenario, the only code you can use is Z68.32 (Body mass index [BMI] 32.0-32.9, adult).
Resource: See the CDC charts on weight and BMI at www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html.
