Part B Insider (Multispecialty) Coding Alert
Give Your Multiple Infusion Reporting A Much-Needed Makeover

Submit one initial service code and primary purpose, not medication sequence, matters most.
Reporting multiple infusions may be routine for you. Oncologists infuse not only chemotherapeutic agents but non-chemotherapeutic agents as well. You should make it a habit to list all infusions and appropriately report each one of them. Here is an example for understanding the reporting of multiple infusions.
Example: You may read that your physician treated a patient with stage IIA non-small cell lung cancer. The patient had a surgical resection followed by four cycles of carboplatin/Taxol. Your physician now documents the patient has metastatic disease to the bone. The physician treats the patient with chemotherapy and non-chemotherapy medications. Chemotherapy was started with pemetrexed (Alimta®) 500 mg/m2 and bevacizumab (Avastin®) 15 mg/kg. Treatment was given every 21 days. The patient also received zoledronic acid (Zometa®) 4 mg IV every 28 days.
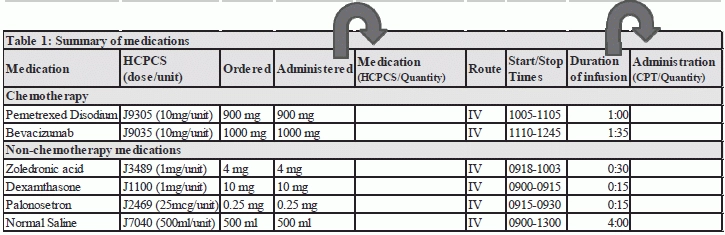
The first step for you is to prepare a summary of the medications the physician ordered and was administered. Note both the chemotherapy and non-chemotherapy medications administered. It is best to prepare clear documentation for how much medication was ordered, how much was administered, the route by which the medication was given and the duration of each infusion. As an example of how you would record the summary of the medications administered, see Table 1. A table such as this may help you better visualize the therapy and coding required. Use the last column to record the administration CPT® codes and quantities.
Code Every Infusion
The physician’s progress note indicates the infusion therapy is to deliver chemotherapy. Therefore, the initial code should be selected for one of the chemotherapeutic medications. Report CPT® code 96413 (Chemotherapy administration, intravenous infusion technique; up to 1 hour, single or initial substance/drug) for the administration of pemetrexed disodium your physician administers over an hour.
Next, turn your attention to bevacizumab. The infusion lasted 1 hour and 35 minutes. For this infusion report CPT® code +96417 (Chemotherapy administration, intravenous infusion technique; each additional sequential infusion [different substance/drug], up to 1 hour [List separately in addition to code for primary procedure]) for the first hour and CPT® code +96415 (Chemotherapy administration, intravenous infusion technique; each additional hour [List separately in addition to code for primary procedure]) for the additional 35 minutes.
NOTE: “In order to use an ‘each additional hour code’ of any kind, the infusion must last 30 minutes beyond the hour (or at least 31 minutes) to support it,” says Kelly C. Loya, CPC-I, CHC, CPhT, CRMA, Director of Reimbursement and Advisory Services, Altegra Health, Inc.
For the non-chemotherapy infusions, report the following codes:
- You should report the 30 minute infusion of zoledronic acid with CPT® add-on code +96367 (Intravenous infusion, for therapy, prophylaxis, or diagnosis [specify substance or drug]; additional sequential infusion of a new drug/substance, up to 1 hour [List separately in addition to code for primary procedure]).
- You should report the 15 minute infusions of palanosetron and dexamethasone given over 15 minutes at separate times with two units of CPT® add-on code +96375 (Therapeutic, prophylactic, or diagnostic injection [specify substance or drug]; each additional sequential intravenous push of a new substance/drug [List separately in addition to code for primary procedure]).
NOTE: “An infusion of 15 minutes or less is reported as an intravenous (IV) push,” Loya says.
According to CPT® guidelines, when administering multiple infusions, injections or combinations, you should report only one initial service code, unless protocol requires that two separate IV sites must be used and is appropriately supported by the documentation. “Choosing the correct initial CPT® when coding infusions can be confusing. You need to know what type of drug is being administered,” says Elizabeth Wernet, CPC, CHONC, Certified Coding Specialist, Healthcare Management Resources, Inc. in Eagan, MN. “The common hierarchy is: Chemo infusions, followed by therapeutic drugs and prophylactic and diagnostic services, and lastly hydration.”
Exception: As noted above, it is appropriate for you to submit two initial codes when administration requires and the doctor documents to include two separate IV sites. The only other exception to reporting more than one initial CPT® administration code is when the patient presents for two different encounters on the same day. “For example, a patient received chemotherapy in the morning and the infusion is complete and patient is discharged from the infusion area,” Loya says. “Later that day the patient calls with a concern or issue. The physician has them return later the same day. As a result of the visit, the physician orders additional supportive medication or hydration to alleviate the acute, unexpected issue. You could bill the separate encounter and initial code again that day with a modifier to describe the situation that occurred and as documented.”
How do you choose the initial service code? When administration codes are reported in a nonfacility setting, you should always report the initial service code that best describes the primary reason why the patient reported to the physician. “In a facility setting, you use the hierarchy algorithm,” Loya says. “Chemotherapy is primary to therapeutic and prophylactic; therapeutic and prophylactic is primary to hydration. You report codes in either setting is irrespective of the order in which the infusions/injections occurred.”
Tip: “As an example, if a patient presents for IV chemotherapy and prior to the chemo, your physician administers a therapeutic drug such as antiemetic medication via IV infusion (20 minutes), you would code the initial code for the chemotherapy infusion followed by a subsequent infusion code for the therapeutic infusion 96413, 96367 plus appropriate HCPCS codes for the drugs,” Wernet says.
Skip incidental hydration: Do not report intravenous fluids provided to patients to facilitate IV access and not given for therapeutic purposes. “The intravenous fluid in this situation would be incidental hydration being used as a vehicle for administration,” Loya says. “When your physician uses saline to administer a medication, you do not report a hydration code. Also [in a nonfacility setting] you do not report the intravenous fluid supply,” Wernet says.
Check routes of administration: You may also check if your physician used multiple routes to administer the medications. “When your physician administers medications using different routes, you follow the sequence of reporting infusions, followed by IV or intra-arterial pushes, and lastly injections,” Wernet says. “For supporting reference, you may find this information clearly described in the CPT® manual in the section preceding the hydration CPT® codes,” Loya says.
Be Precise with Units for HCPCS Codes
Report the HCPCS codes for both the chemotherapy and non-chemotherapy medications.
For pemetrexed and bevacizumab, you report the following J codes:
- J9305, Injection, pemetrexed, 10 mg
- J9035, Injection, bevacizumab, 10 mg
- For the non-chemotherapy medications, you submit the following J codes:
- J1100, Injection, dexamethasone sodium phosphate, 1mg
- J2469, Injection, palonosetron HCl, 25 mcg
- J3489, Injection, zoledronic acid, 1 mg
To ensure payment for the entire amount of drug your physician administered, you need to report the accurate numbers of units for the medications. “Because some drugs are quite expensive and also toxic, treatment protocols are determined and only a particular number of units of the drug may be allowed,” Wernet says. “This is where the medically unlikely edits (MUE) come into play. If you bill an excess of units you most likely will receive a MUE denial, as the payer will recognize too large of the quantity of the drug was billed.”
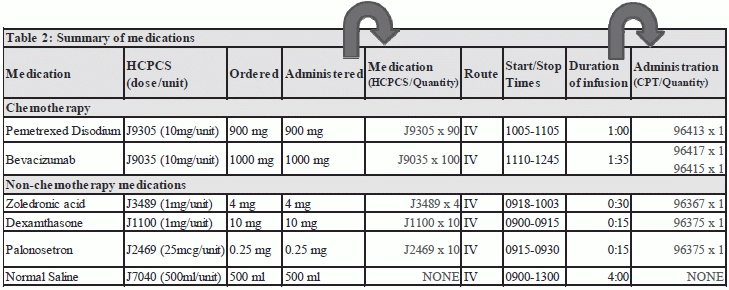
You report 90 units of J9305 for pemetrexed as one unit of J9305 covers 10 mg of pemetrexed. The documentation supports 900 mg of pemetrexed administered, or 90 units of J9305. Similarly, you calculate the units of J9035 for bevacizumab. You submit 100 units of J9035 for 1000 mg of bevacizumab that was administered. One unit of J9035 equals 10 mg of bevacizumab.
One unit of codes J1100 and J3489 is reported for every 1 mg of dexamethasone and zoledronic acid, respectively. Since your physician administers 10 mg of dexamthasone and 4 mg of zoledronic acid, submit 10 units of J1100 and 4 units of J3489.
Lastly, one unit of HCPCS code J2469 reports 25 mcg of palonosetron hydrochloride. Since 0.25mg was administered, of palonosetron, you would submit 10 units of J2469. You do not report any HCPCS code for saline as this is incidental hydration. (Table 2 illustrates the codes and quantities from the above example).
Part B Insider (Multispecialty) Coding Alert
- Part B Revenue Booster:
Stop Repeatedly Making This $35 Mistake
Document your discharge services properly or you’ll be forced to downcode. How much time does [...] - Injection Coding:
Study These 5 Injection FAQs to Perfect Your Accuracy
From pain management injections to TB testing, we’ve got your answers. Although performing injections might [...] - Compliance:
Watch Out For Sophisticated Malware Breaching Your Systems From Overseas
Pay attention: Massive breach teaches you four crucial lessons. The latest HIPAA breach is the [...] - Part B Coding Coach:
Give Your Multiple Infusion Reporting A Much-Needed Makeover
Submit one initial service code and primary purpose, not medication sequence, matters most. Reporting multiple [...]

