Part B Insider (Multispecialty) Coding Alert
Follow These 5 Tips to Improve Your Endoscopic Injection Income

Don’t miss opportunities to code multiple injections despite restrictions.
If you include an injection as part of the endoscopy code when your gastroenterologist administers them during the procedure, you may be losing precious dollars for your practice.
With so many options for injectables as well as diseases that your physician can treat with injections, it’s essential that you know which codes are available for these injections.
Plus, as the injections provided by your GI may be for different purposes, you have to know how to differentiate between a therapeutic injection and an injection given for destruction of lesions so that you don’t miscode the situation. Capture the max revenue for your physician’s injection services by following these five golden rules.
1. Type of Endoscope Decides the Injection Code
CPT® has provided dedicated injection codes when the physician inspects the submucosal area during upper or lower GI endoscopy and injects a therapeutic drug. The physician may also use a submucosal injection to mark a lesion (with a substance such as India Ink) or lift a lesion for easier removal.
Upper GI: If your physician performs an upper endoscopy with injection, you have an option to report one of the following codes:
-
43192 -- Esophagoscopy, rigid, transoral; with directed submucosal injection(s), any substance
-
43201 -- Esophagoscopy, flexible, transoral; with directed submucosal injection(s), any substance
-
43236 -- Esophagogastroduodenoscopy, flexible, transoral; with directed submucosal injection(s), any substance.
You should report 43236 for “submucosal saline injections (as with endoscopic mucosal resection or polypectomy), botulinum toxin injection (for achalasia), India ink (for tattooing), steroid injection, or any other substance, excluding a sclerosant for esophageal/gastric varices or epinephrine to control bleeding.” Look at the extent of the scope travelled to decide if the procedure was an esophagoscopy (43201) or an EGD (43236). “Injections to help with mucosal resections may contain other substances with saline like methylene blue or hyaluronic acid that help define the edges of the polyp to be removed,” informs Michael Weinstein, MD, Vice President of Capital Digestive Care. “Coding with these substances is no different,” he adds.
Hint: Endoscopy that includes the duodenum or jejunum as part of the examination is an EGD.
Lower GI: If your general physician performs a lower endoscopy with an injection, you’ll instead report one of the following codes, based on whether the physician performs a sigmoidoscopy or colonoscopy:
-
45335 -- Sigmoidoscopy, flexible; with directed submucosal injection(s), any substance
-
45381 -- Colonoscopy, flexible; with directed submucosal injection(s), any substance
-
44404 -- Colonoscopy through stoma; with directed submucosal injection(s), any substance.
Caution: According to the CPT® guidelines, you should not separately report these injection codes in conjunction with control of bleeding and endoscopic mucosal resection codes for the same lesion and location.
2. Stay Away From Injection Codes for Sclerotherapy
Other than marking or therapeutic reasons, one other common use for administering an endoscopy with injection is for sclerotherapy (destruction of varices). In such cases, however, you should forget the injection codes altogether and opt for the sclerosis/destruction codes instead. Same rules of location apply here as did for injections. Therefore, you should report:
-
43204 (Esophagoscopy, flexible, transoral; with injection sclerosis of esophageal varices), if the GI destroys varices in an esophagoscopy;
-
43243 (Esophagogastroduodenoscopy, flexible, transoral; with injection sclerosis of esophageal/gastric varices).
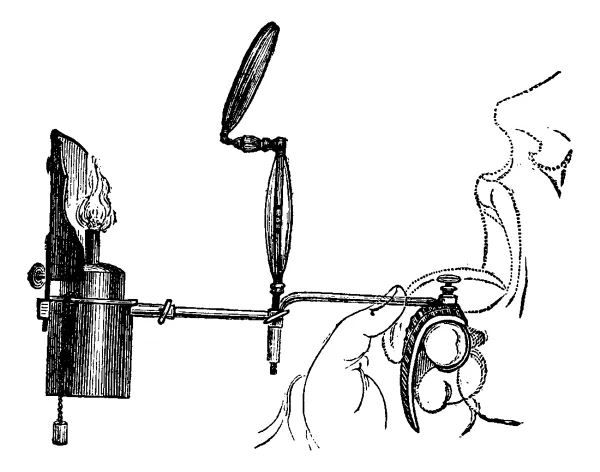
A variety of substances can be injected into the submucosal space of the digestive tract through a sheathed needle-tipped catheter inserted through an endoscope. One of the first applications of this technique was the use of sclerotherapy to control variceal hemorrhage. Due to the success of sclerotherapy, endoscopists expanded their scope of injections and found that injection of nonsclerosing substances, such as diluted epinephrine and saline, was helpful in controlling bleeding from nonvariceal sources, such as peptic ulcers.
Bottom line: Be sure not to use the injections for sclerotherapy codes when you are injecting other substances.
3. Get Paid for Injections for Separate Procedures
There are times when your physician will perform an endoscopy with injection procedure during the same session as another procedure. These codes can often be used in combination with other codes as long as there is clear documentation.
Example: If your physician performs a polypectomy (such as 45385, Colonoscopy, flexible; with removal of tumor[s], polyp[s], or other lesion[s] by snare technique) and tattooing for subsequent resection (45381-45359) during the same session, you can report both procedures.
Example 2: Sometimes, the physician may inject the base of a polyp with saline (45381), and then remove the polyp by snare in piecemeal fashion (45385). The physician will then inject India ink at the polypectomy site to be able to identify the location in the future. You can report this injection procedure with codes 45381.
4. New Endoscopic Mucosal Resection Codes Include Injections
In 2014, new CPT® codes were added for Endoscopic Mucosal Resection in the upper GI tract; and in 2015, new CPT® codes were added for the lower GI tract and EMR. “These codes include the injections that are performed to assist the EMR procedure so do not bill these injections separately,” Weinstein says. The new codes are:
-
45385 -- Esophagoscopy, flexible, transoral; with endoscopic mucosal resection
-
43254 -- Esophagogastroduodenoscopy, flexible, transoral; with endoscopic mucosal resection
-
45349 -- Sigmoidoscopy, flexible; with endoscopic mucosal resection
-
45390 -- Colonoscopy, flexible; with endoscopic mucosal resection.
5. Coding Control of Bleeding Separately is Possible
You can separately report codes for hemostasis (control of bleeding) separately if the bleeding is the reason the procedure is being performed. According to CPT® guidelines, when your physician uses injection therapy to “control hemorrhage not associated with esophageal or gastric varices,” you can report either of codes 43227 (Esophagoscopy, flexible, transoral; with control of bleeding, any method) or 43255 (Esophagogastroduodenoscopy, flexible, transoral; with control of bleeding, any method).
Take a breath: However, if the bleeding is the result of a diagnostic or therapeutic intervention, you should strictly forego the hemostasis codes unless it happens at a separate session. If there is indeed a separate session and the control of bleeding is separately reportable, append modifier 59 (Distinct procedural service).
Related Articles
Part B Insider (Multispecialty) Coding Alert
- Part B Revenue Booster:
Can A Typo Cost You Tens of Thousands?
Yes it can, this billing pro says. With 2016 right around the corner, now is [...] - Teaching Physicians:
CMS Offers 2 Telehealth Examples for Teaching Physicians
Get to the bottom of when you can—and cannot—report telehealth to Part B. As long [...] - Cardiology:
Check Out These New, Revised 2016 HCPCS Codes to Keep Your Income Flowing
Plus: Get Varithena coding tips from the HCPCS committee preliminary decision. With all the fanfare [...] - Reader Question:
Don't Change POS for SNF Patient in Office
Question: Thank you for your recent article about audits on E/M services performed in SNFs (Insider [...] - Part B Coding Coach:
Follow These 5 Tips to Improve Your Endoscopic Injection Income
Don’t miss opportunities to code multiple injections despite restrictions. If you include an injection as [...] - Physician Notes:
EHR Incentive Payments Are Valuable--But Not This Valuable
Plus: RACs could face limits very soon. Medical practices and facilities that used electronic health [...]