3 Tips Lead You to Successful Spirometry Claims

Spirometry is one of the most frequent diagnostic tests used by pulmonologists to confirm various pulmonary diseases. However, you need to remember two things while reporting the diagnostic codes to support it: specificity and medical necessity.
Background: Pulmonologists use spirometry (94010, Spirometry, including graphic record, total and timed vital capacity, expiratory flow rate measurement[s], with or without maximal voluntary ventilation; and 94060, Bronchodilation responsiveness, spirometry as in 94010, pre- and post-bronchodilator administration) to measure how quickly the patient’s lungs can move air in and out, as well as how much.
The patient breathes into the mouthpiece of a tube connected to the spirometer, which measures the airflow. The procedure is useful to detect obstructive airway diseases, such as asthma and chronic obstructive pulmonary disease (COPD).
1. Negate Payer Rejection With the Highest Code Specificity
Although the payment for spirometry tests is based on the CPT® codes you report and not on the diagnosis, the payer can easily reject your claim if you can’t establish a credible medical necessity for the procedure by applying the correct diagnosis code. These ICD-9 or ICD-10 codes inform the payer why the pulmonologist had to perform the spirometry. Increasingly, carriers deny payment if the diagnostic codes are not specific enough.
Ensure that you are coding to the highest possible level of specificity by collecting complete information. While you are converting the physician’s encounter information into codes, you need to have complete information at your hands.
For example, if the doctor simply writes “chronic bronchitis” in the patient’s record, you need more information. Chronic bronchitis is a very non-specific diagnosis and most likely to be denied because of missing digits. ICD-9 classifies Chronic bronchitis under the parent family code 491 (Chronic bronchitis). Similarly, chronic bronchitis can be reported in ICD-10 through either of the codes J41 (Simple and mucopurulent chronic bronchitis), J42 (Unspecified chronic bronchitis), or J44 (Other chronic obstructive pulmonary disease) family of codes. You need determine the type of chronic bronchitis (simple, mucopurulent, with/without exacerbation, etc.) and whether it is a confirmed diagnosis. Consequently, you will have to seek out more information on the specific symptoms from the patient’s chart or by querying the physician. Specific diagnosis coding requires clear access to all the necessary information.
Use the code with the highest specificity: No matter how well the pulmonologist communicates the patient data, you must ensure that you use the right code and that it is being carried to the highest digit possible. This involves not only noting any caution or warning symbols in the ICD-9 or ICD-10 manual (some color-coded books use yellow for nonspecific codes and red for those with missing digits) but also having a good working knowledge of the terminology associated with spirometry. From the example above, if the physician sees a patient for chronic bronchitis, you will have to support the diagnosis codes by gathering enough information to know that the patient has obstructive chronic bronchitis with acute exacerbation.
Find the correct and complete code under chronic bronchitis with acute exacerbation (491) in the ICD-9 system and similarly in the ICD-10 manual (J41, J42, J44). The simple rule is: Assign higher-level codes only if there are no sub-codes within that code category. For example, assign four-digit codes only if there are no fifth-digit sub classifications for that category. Otherwise, assign the closest fifth-digit sub classification code for those categories where it exists.
In our earlier example, the specific ICD-9 code to report is 491.21 (Obstructive chronic bronchitis with [acute] exacerbation). The fourth digit indicates that there is an element of COPD present, and the fifth digit clarifies that there is an acute exacerbation of the chronic condition. Under ICD-10, the appropriate code would be J44.1 (Chronic obstructive pulmonary disease with [acute] exacerbation)
Although carrying out to the fifth digit is mandatory, you occasionally have to use an unspecific code if no code exists that matches the pulmonologists’ documentation. For example, for unspecified chronic bronchitis, you can always report J42 under ICD-10. “J42 may not be considered “medically necessary” for reimbursement, depending upon the payer’s policy,” informs Carol Pohlig, BSN, RN, CPC, ACS, Senior Coding & Education Specialist at the Hospital of the University of Pennsylvania. It is always best to education the physician about the increased documentation requirements for ICD-10, and increased specificity in payer policy requirements,” she adds.
2. Ramp up Your Reports for Error-Free Billing
You can stay updated with the latest diagnosis coding by evaluating your regular code reports. As a good practice, you should generate a report of the top 50 diagnosis codes and top 50 CPT® codes each physician used after every two months. Carefully review the reports, noting which nonspecific codes the pulmonologists used and how often. Report this information to the physicians and keep track of each report to benchmark progress and trends.
In addition, updating your encounter forms occasionally is always beneficial for your practice. This should eliminate the potential for using outdated or deleted codes. Your physicians will also be able to choose diagnoses that reflect their current patient population. Pulmonary physicians are frequently unaware of the many diagnostic codes available to them. They only see the small sample presented to them on their billing slip, and many limit their selection to these codes.
You should ensure including all applicable diagnosis codes on the encounter form to give the doctor the full range of options. This is all the more important now as the vastly expanded ICD-10 nomenclature comes into effect from October. If you only include those codes your carriers have indicated as showing medical necessity, you could be accused of coding for payment, which can be deemed fraudulent.
3. Last Port of Call is Local Policies
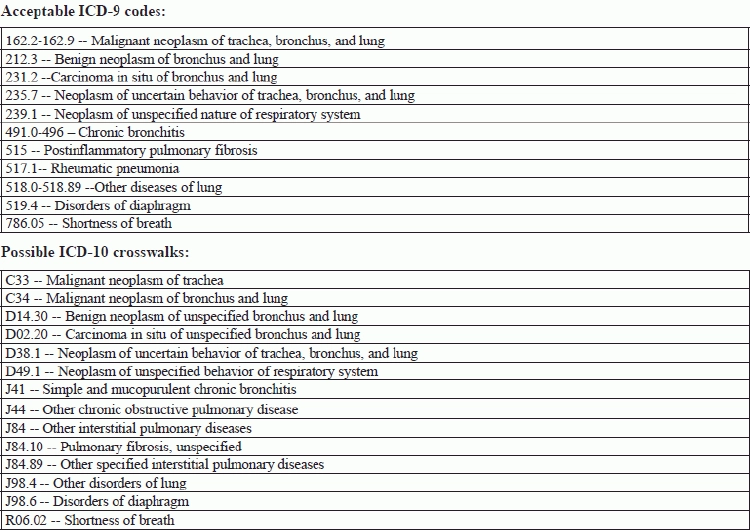
Medicare carriers assign each CPT® code a list of diagnosis codes, which according to them show medical necessity for performing the service. The table below lists the most commonly accepted ICD-9 diagnoses and their possible ICD-10 crosswalks for spirometry. Although these are the most frequently allowed ICD-9 codes, each payer has its own take on the codes.
Consequently, you should contact your carriers and get their policies in writing regarding medical necessity for spirometry. You can use them to ensure that the diagnosis you assign will support your pulmonologist’s decision to use the procedure.
However, you should keep in mind that you cannot just pick a diagnosis from the carrier’s policy because it has stated that it will get paid. You must assign diagnostic codes based on the physician’s documentation. Otherwise, you could be an auditing target for deliberately using paying codes.