Avoid a 4% Penalty — Report MIPS 2017 Data Before March 31
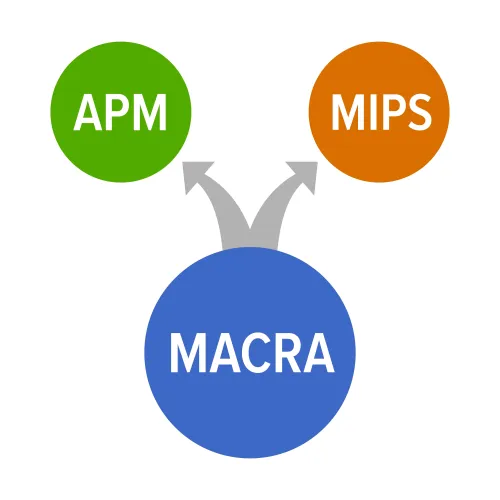
Remember you only need report 90 days of data for 2017 to sidestep penalties. Performance Year 1 of MACRA's Quality Payment Program (QPP) ended on Dec. 31, 2017, but there's still time to submit your data to ensure a positive payment adjustment - as long as you began collecting and submitting measures by Oct. 2, 2017. Review These Pick-Your-Pace Basics For the inaugural year of the Merit-Based Incentive Payment System (MIPS), CMS allowed eligible clinicians to report under its "Pick-Your-Pace" plan. This option gave providers the opportunity to report as much or as little as they wanted. Here is a quick overview of the Performance Year 1 categories and the rewards or penalties for each: Status check: Remember, that if you didn't meet the MIPS participation requirements, you are excluded from the program for Performance Year 1 and off the hook to report any measures for 2017. "Currently, if a clinician or group does not meet both the Medicare revenue and number of Medicare patients' thresholds, the clinician or group is excluded from MIPS and does not have the option to participate," reminds attorney Benjamin Fee, Esq. of Dorsey and Whitney LLP in the Des Moines, Iowa office. Here are the baseline essentials for reporting your MIPS measures for 2017: Deadline: Whether you started sending your data on Jan. 1 or Oct. 2 of 2017, you have until March 31, 2018 to submit and finalize your 2017 performance data under the four MIPS categories. For Performance Year 1, reporting clinicians receive a score in three out of the four categories, which CMS weights according to the relative importance assigned to each, to arrive at a single score between 0 and 100. Take a look at this quick refresher of what constitutes "Partial" or what CMS suggests most MIPS 2017 participants will submit: Resource: For more in-depth information about performance data requirements, how to report your measures before the March 31, 2018 deadline, and CMS guidance, visit https://qpp.cms.gov.




