Next year will be an exciting time for providers who depend on office and other outpatient E/M codes as the bread and butter of their Medicare payments. Starting on Jan. 1, 2021, you can expect substantial changes in the way you code new and established patient office visits.
Plus, you’ll lose code 99201 and put special emphasis on medical decision making (MDM) and time in your provider’s documentation.
“I’m excited about the E/M changes,” says Marcella Bucknam, CPC, CCS-P, COC, CCS, CPC-P, CPC-I, CCC, COBGC, revenue cycle analyst with Klickitat Valley Health in Goldendale, Washington. “These changes are going to address several long-standing problems with E/M coding and I’m excited that Medicare and the AMA are finally getting on the same page.”
Read on to learn more about how your office/outpatient visit coding will change starting in 2021.
Review Revisions for 99202-99205
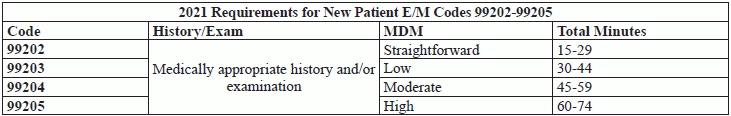
Currently, for the new patient office or outpatient codes (99202-99205), you use three key components — history, examination, and MDM — to select the appropriate E/M service level. But, starting on Jan. 1, 2021, CPT® will remove history and exam as key components for 99202-99205 for new patients. Instead, your code selection will be based upon the MDM level or the total time the provider spent with the patient on that date of service. This change also applies to office codes (99212-99215) for established patients. Additionally, CPT® will update and revise their guidelines, which will further explain how coders should handle MDM and time in 2021.
However, this change does not mean that providers should not perform a history and exam, experts say.
The provider should obtain a medically relevant history and exam, says Rae Jimenez, CPC, CIC, CPB, CPMA, CPPM, CPC-I, CCS, senior vice president of product at AAPC and coding liaison to the AMA CPT® Editorial Panel. Although history and exam will not be factored into choosing the E/M level, they are still an important part of the medical record. It is up to the physician’s clinical determination of what level needs to be performed and documented.
Example: Take a look at the revised code descriptor for 99202 to get an idea of how these changes will be reflected:
So, as you can see, the revised descriptor for 99202 explains the level of MDM — straightforward. The descriptor for 99202 also specifies what the time should have been — 15-29 minutes of total time spent on the date of the encounter — if this was the determining factor for the E/M level. And, the revised descriptor describes “a medically appropriate history and/or examination.”
All the new outpatient patient codes (99202-99205) follow this same structure. To get a better idea of the requirements for revised codes 99202-99205, review the handy chart below.
Scenario: Your neurosurgeon meets a new patient in his office who presents with severe headaches. The neurosurgeon spends 30 total minutes with the patient on the date of service. The neurosurgeon also performs a medically appropriate history and exam during the encounter. You should report 99203 for this service.
Say Goodbye to 99201 in 2021
Reminder: In 2021, you won’t be able to use 99201 because CPT® will delete this code.
Take a look at the current code descriptors for 99201 and 99202:
Since both 99201 and 99202 require “straightforward MDM,” having both codes with the same level of MDM would be unnecessary. So, AMA will delete 99201, and this was approved by CMS in the Final Rule.
“Code 99201 is a code seldom used by physicians, so removing this code makes sense,” says Arnold Beresh, DPM, CPC, CSFAC, in West Bloomfield, Michigan.
