Hint: Your best coding starts with a detailed diagnosis.
If your practitioner treats a patient for dysphagia (difficulty in swallowing), catching all the details will make the difference in your coding. Read on for our experts’ advice on making the correct choices.
1. Know What to Watch for In Exam
“Actually the best coding starts with a detailed history and exam,” says Cheryl Odquist, CPC, CPC-I, senior coding and documentation specialist for Scripps Health in San Diego, Cal.
History: “It’s important to note whether the problem is difficulty swallowing or pain on swallowing (odynophagia),” Odquist says. “Dysphagia to solids suggests esophageal or other structural obstruction. Dysphagia to liquids suggests pharyngeal disorders, including neuromuscular disease.” Weight loss in a patient with dysphagia is an indicator of the significance and duration of the disease. Other important history components to check the provider’s documentation for include a history of voice changes, hemoptysis, regurgitation of food, nasal leakage of liquids, otalgia, any ingestion of caustic substances, and previous surgery or trauma of the pharynx, chest, or abdomen.
Review of systems: This portion of the exam often reveals systemic diseases that cause dysphagia. Use of certain medications such as antihistamines, anticholinergics, antidepressants, and antihypertensives can affect salivary gland function or the neurology of swallowing. Systemic neuromuscular or autoimmune disorders may cause problems with esophageal motility. A family history of digestive diseases such as oculopharyngeal dysphagia or muscular dystrophy can also be clues to the patient’s condition.
Physical examination: Notes from the provider’s physical examination should be quite detailed in order to thoroughly document the patient’s condition. Patients with dysphagia can experience wheezing or labored breathing (respiratory), changes in voice quality, a gurgling noise in the neck, or thick mucoid or foamy secretions in the pirifom sinus or laryngeal vestibule. Your provider should also document observations of vocal fold movement, symmetry of the pharyngeal constrictors, and arytenoids immobility.
2. Discover the Best Diagnosis
The code family for a dysphagia diagnosis is 787.2x (Dysphagia). The fifth digit represents the condition’s phase so you can better report the patient’s status. Your choices are:
Oral, pharyngeal and esophageal are the three phases of swallowing, which is why the diagnosis codes are distinguished in this manner.
Quick fact: Physicians normally direct patients who complain about any type of upper throat swallowing problem to a speech-language pathologist (SLP) for an appropriate swallow evaluation. SLPs are the ones who actually definitively diagnose dysphagia, determine what type, and develop a treatment plan.
You’ll also want to include any pertinent diagnoses related to what caused the patient’s dysphagia. Odquist shares a few common examples of what might cause dysphagia:
3. Evaluate the Services Provided
CPT® includes six codes representing dysphagia treatment services which usually involve the SLP’s participation:
Profit: The Medicare rate for dysphagia treatment (92526) is about $77 (based on a non-facility RVU of 2.27 and the 2013 national conversion factor of $34.023).
4. Keep an Eye on CCI Bundles
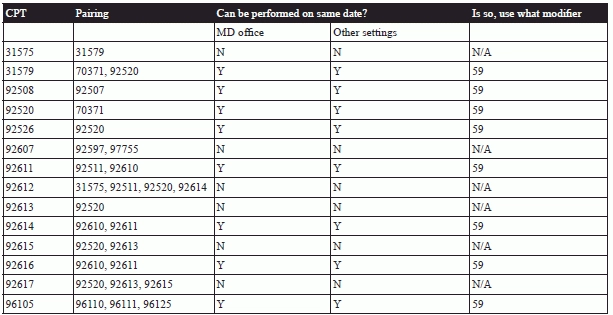
Correct Coding Initiative (CCI) edits bundle quite a few procedures with 92526, meaning you need to take care before reporting multiple services provided on the same day.
Possible reporting: Other coding bundles, however, allow you to report dysphagia treatment with some other services when you have clear documentation that the two services were separate and distinct from each other. For example, you cannot report 92612 on the same day as 92614. However, CCI edits do allow billing 92610 on the same day as 92611, provided you have adequate documentation of the separate services and append modifier 59 (Distinct procedural service).
Check out some of the other dysphagia-related pairings included in CCI edits: