These ICD-9 Tips Will Improve Your Histoplasmosis Coding Accuracy
Ignoring symptoms could cost you $172.
Reporting diagnoses for histoplasmosis patients can be like walking a tight rope, because you may find that although your patients are symptomatic, they are relatively free of any ill effects from the affliction. If the pulmonologist makes even the slightest omission in documenting the accurate respiratory symptoms, you might find your claim denied by your insurer.
Background: Histoplasmosis (115.xx), also called as Darling’s disease, is caused by the dimorphic fungus, Histoplasma capsulatum. The disease is caused by breathing in spores from the fungus found in bat or bird droppings. The fungus gets dispersed in the environment through the air and when susceptible persons inhale this fungus, it enters the lungs. The lungs are the primary site of infection although secondary infection may spread to other organs too, in which case this disease is classified as disseminated histoplasmosis (i.e., 115.01, Histoplasma capsulatum meningitis, and 115.02, Histoplasma capsulatum retinitis), such as in immunocompromised patients (AIDS). After the ICD-10 transition, you will report B39.- (Histoplasmosis) for the condition.
We will review a case to give you stepwise guide to reporting histoplasmosis and its treatment:
A 57-year-old man presents to the pulmonologist with symptoms of chronic dry cough, loss of weight, chest pain, and expectoration. The pulmonologist conducts an examination, including an extensive history and physical, and the review of the patient’s medical records. The patient informs that he has been cleaning and renovating an old and abandoned bird coop on his farm land. She then orders a fresh chest x-ray and a complete blood test. As the symptoms are ambiguous, she also performs skin tests to confirm histoplasmosis and rule out tuberculosis.
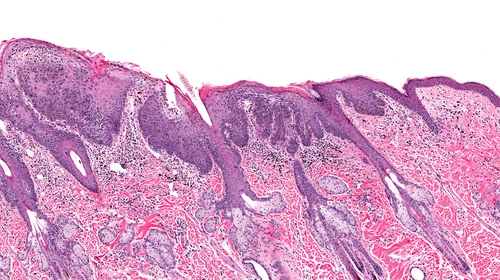
Skin test basics: The provider cleans an area of the patient’s skin, usually the forearm. She then injects a concentration of tuberculin purified protein derivative (PPD) or an allergen just below the cleaned skin surface. The provider checks the injection site at 24 hours, 48 hours, and at 72 hours for signs of a reaction. Occasionally, the reaction may not appear until the fourth day.
She schedules the patient for a follow-up visit after two days to interpret the test results and perform a more extensive diagnostic workup. How should you report this encounter?
Symptoms Rule the Roost in Deciding Histoplasmosis
There may be varying presenting symptoms of histoplasmosis. Most people have no symptoms, or only have a mild flu-like illness. However, if symptoms do occur, mostly it is a combination of the following:
Wisely Pick the Tests You Can Report
If you are reporting the blood tests the physician ordered, your claim could already be doomed. “Only the pathology lab will bill the blood test, not the pulmonologist. Your physician will only document her personal review of the lab report in the progress notes and provide the appropriate diagnosis coding with the lab order so that the lab analyzing the specimen can get paid, and the patient does not bear the expense,” says Carol Pohlig, BSN, RN, CPC, ACS, Senior Coding & Education Specialist at the Hospital of the University of Pennsylvania. In this case, the ICD-9 codes supporting medical necessity of the lab test are chronic dry cough (786.2), expectoration (786.9), and chest pain (786.50).
Because the physician performed the tuberculosis and histoplasmosis skin tests, you can report this service with 86580 (Skin test; tuberculosis, intradermal) and 86510 (Skin test; histoplasmosis). For the TB test, you may claim $7.87 (0.22 RVUs multiplied by the 2015 conversion factor of 35.7547). Your office can also expect a payment of $6.18 (Medicare) or $6.07 (Others) in reimbursement (0.17 RVUs multiplied by the 2015 conversion factor of 35.7547) for the histoplasmosis skin test.
Note: “Code 86510 and 86580 both include the Histoplasma antigen injection. Don’t separately report an administration code such as 96372 (Therapeutic, prophylactic, or diagnostic injection [specify substance or drug]; subcutaneous or intramuscular) with 86510,” warns Pohlig.
Sometimes, your physician may also order specific histoplasmosis antibody tests or a biopsy of the lung tissue to confirm severity of histoplasmosis. Again, if the lab conducts the enzyme immunoassay tests, you cannot report codes such as 86698 (Antibody; histoplasma) or 87385 (Infectious agent antigen detection by enzyme immunoassay technique, qualitative or semiquantitative, multiple-step method; Histoplasma capsulatum). However, if your office performs the bronchoscopy w/ biopsy, then you can report the service with 31628 (Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with transbronchial lung biopsy[s], single lobe) or 31632 (Bronchoscopy, rigid or flexible, including fluoroscopic guidance, when performed; with transbronchial lung biopsy[s], each additional lobe [List separately in addition to code for primary procedure]).
Track Your E/M Time
You should bill the initial encounter using E/M codes for office visits (99201-99205), which includes the three key components history, exam and medical decision-making. In the discussed case, you will likely choose 99204 (Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components:…) due to the comprehensive history and exam, the lengthy medical-record documentation that the pulmonologist reviewed, and the complexity of the diagnostic workup required to confirm the diagnosis.
You should expect to get about $165.90 for reporting 99204 (4.64 RVUs multiplied by the 2015 conversion factor of 35.7547). Even for Medicare, you must report a new (99201-99205) or established (99212-99215) patient visit, depending on whether the patient has been seen by anyone in the group (and specialty) within the last three years in any setting (inpatient or outpatient). Your payer will probably request that you append modifier 25 (Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service) to your E/M claim.
Align Follow-Up Reporting With Provided Services
In the discussed case, the pulmonologist sees the patient after two days. After reading the results of the skin and blood tests, the pulmonologist confirms that the patient has acute pulmonary histoplasmosis. The doctor spends 30 minutes with the patient reviewing the test results and counseling him on the risks of continued exposure to contaminated soil. The doctor may decide against any treatment if the patient’s symptoms are mitigated or may prescribe him an antifungal medication (e.g., Itraconazole). She may advise the patient to stay away from the farm to avoid further exposure.
Code it: You could choose from any of the established patient visit codes (99211-99215). For this particular scenario, you’ll most likely report 99214 (Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: A detailed history; A detailed examination; Medical decision making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem[s] and the patient’s and/or family’s needs. Usually, the presenting problem[s] are of moderate to high severity. Physicians typically spend 25 minutes face-to-face with the patient and/or family.). Then, you should link 115.05 (Histoplasma capsulatum pneumonia) with 99214 to represent the confirmed diagnosis.
Do not bill 86510 again when the patient returns for the reading of the test results. You should also keep from billing another office visit if the only service that occurs during the follow-up is the histoplasmosis skin test reading. Although some payers may permit billing a minimal E/M (e.g., 99211) for the reading, the patient may be required to pay a co-pay for this service.
Alternative: If the patient returns to the office, has the skin test read, and requires an E/M service for counseling or to institute treatment, or for a different problem, then that’s the time you should report the appropriate diagnosis and E/M code.