Part B Insider (Multispecialty) Coding Alert
Get Ready for Revamped Office/Outpatient Consultations Codes in 2023
Factor in updated descriptions as well as using MDM versus time.
You can get ahead of the curve by studying the evaluation and management (E/M) service code changes for 2023 before they go live on January 1.
First, you’ll need to adopt the same medical decision making (MDM) and time changes for other E/M services as the ones CPT® introduced in 2021 for 99202-99205/99211-99215 office/ outpatient E/M services. Among the categories to which guideline, headline, and code revisions will apply on Jan. 1, 2023, are the office/outpatient consultation codes.
Read on for the details.

Add 2021 E/M Rules to Consultations in 2023
The changes begin with revisions to the consultation CPT® guidelines, including adding “other qualified healthcare professional” to the providers who will be able to perform consultations as well as start diagnostic or therapeutic services during the visit or at a subsequent visit.
CPT® has also revised the places of service where consultations can take place in the 2023 code set:
- CY 2022: “…report consultations provided in the office or in an outpatient or other ambulatory facility, including hospital observation services, home services, domiciliary, rest home, or emergency department.”
- CY 2023: “…report consultations that are provided in the office or other outpatient site, including the home or residence, or emergency department.”
Mandatory modifier: The guidelines also state that you should append modifier 32 (Mandated services) to a consultation that is required. For example, if a payer requests a consultation, such as a second opinion before the payer approves treatment, you should append modifier 32 to the applicable consultation code.
Know the Revised Office/Outpatient Consultation Codes
CPT® has also updated the office/outpatient consultation codes to allow the provider to select the level visit based on MDM or time when applicable.
The revised office/outpatient consultation E/M codes for CY 2023 are as follows (Note: Portions of the revised descriptors are emphasized for easy reference):
- 99242 (Office or other outpatient consultation for a new or established patient, which requires a medically appropriate history and/or examination and straightforward medical decision making. When using total time on the date of the encounter for code selection, 20 minutes must be met or exceeded.)
- 99243 (Office or other outpatient consultation for a new or established patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using total time on the date of the encounter for code selection, 30 minutes must be met or exceeded.)
- 99244 (Office or other outpatient consultation for a new or established patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using total time on the date of the encounter for code selection, 40 minutes must be met or exceeded.)
- 99245 (Office or other outpatient consultation for a new or established patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using total time on the date of the encounter for code selection, 55 minutes must be met or exceeded.)
Add on this prolonged service code: CPT® 2023 also adds a parenthetical note to 99245 instructing you to use prolonged services add-on code +99417 (Prolonged outpatient evaluation and management service(s) time with or without direct patient contact beyond the required time of the primary service when the primary service level has been selected using total time, each 15 minutes of total time (List separately in addition to the code of the outpatient Evaluation and Management service)) for services lasting 70 minutes or longer.
If you’re billing an office/outpatient consultation E/M visit solely on the basis of time, you can assign +99417 only after 15 minutes have elapsed beyond the initial 55 minutes of the 99245 consultation — in other words, after the service has exceeded 70 minutes total time. Additionally, the 15 minutes of +99417 may count whether the provider was in direct contact with the patient or not.
Key code deletion: CPT® 2023 deletes 99241 (Office consultation for a new or established patient, which requires these 3 key components: A problem focused history; A problem focused examination; and Straightforward medical decision making…). Instead, you’ll report 99242 for a consultation that involves straightforward MDM.

Understand How to Choose the Correct Consultation Code
“As part of the 2023 revisions, this range of consultation codes can be documented through either time or MDM. History and exam, as with office visits, are no longer key components of consultations,” says Nancy Clark, CPC, COC, CPB, CPMA, CPC-I, COPC, AAPC Fellow, senior manager at Eisner Advisory Group LLC in Iselin, New Jersey.
Going forward on Jan. 1, 2023, you’ll use either documented time or MDM to support your E/M consultation code choice. You should review your individual payer preferences, but if they don’t have specific additional requirements, you, along with provider documenters, can decide how to support your code choice for the encounter. Provider documenters are the providers who document and select the code.
What if you have a report that states the provider used a certain level of MDM, but the total time surpassed a higher level of MDM? “If the provider documents cumulative time along with the MDM and relevant history/physical examination, the coder can select the method that benefits the provider,” says Carol Pohlig, BSN, RN, CPC, manager of coding and education in the department of medicine at the Hospital of the University of Pennsylvania in Philadelphia.
The same applies to provider documenters. The provider has the ultimate responsibility to document and select the code. “If the provider believes the encounter was especially lengthy, they may choose to document the time spent in various activities and select a code based on time,” Clark adds.
Example: A physician performs an E/M visit where the documentation supports moderate complexity MDM (99244), but the total time for the visit is 55 minutes (99245). In this case, you can assign 99245 for the service.
Related Articles
Part B Insider (Multispecialty) Coding Alert
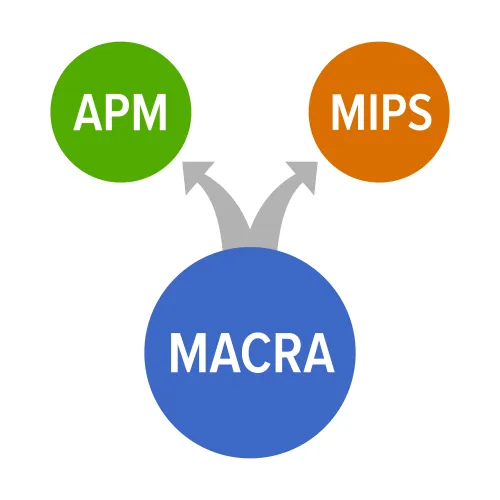
- Quality Payment Program:
Get a Grip on MIPS Proposals for 2023
CMS plans a slow rollout for MVPs. If last year’s finalized overhaul of the Merit-Based [...] - CPT® 2023:
Get Ready for Revamped Office/Outpatient Consultations Codes in 2023
Factor in updated descriptions as well as using MDM versus time. You can get ahead [...] - Part B Coding Coach:
Cut Duplicate Claims With This Expert Insight
Tip: Review the basics on repeat modifiers to decrease denials. If Medicare denials are piling [...] - Reader Questions:
Check Out the Rules on Extended Repayment Schedules
Question: Our Part B practice made a major billing error that resulted in a massive overpayment [...] - Reader Questions:
Understand the Right of Access Provision to Avoid HIPAA Issues
Question: One of our patients has a sizable balance and hasn’t responded to requests for payment. [...] - Physician Notes:
Know the Facts on Medicare Provider Enrollment and Revalidations
As the healthcare industry continues to reinstate policies as COVID cases ebb and flow, you [...] - Physician Notes:
Pocket These Critical Details on the Accelerated Payment Recoupment Process
If you intend to submit a debt dispute over COVID-19 Accelerated and Advance Payment (CAAP) [...] - Physician Notes:
Feds Open MIPS 2021 Targeted Review Window
If your MIPS data, final score, or payment adjustment for the 2021 performance year doesn’t [...]