Don't Forget Negative Responses in ROS Documentation
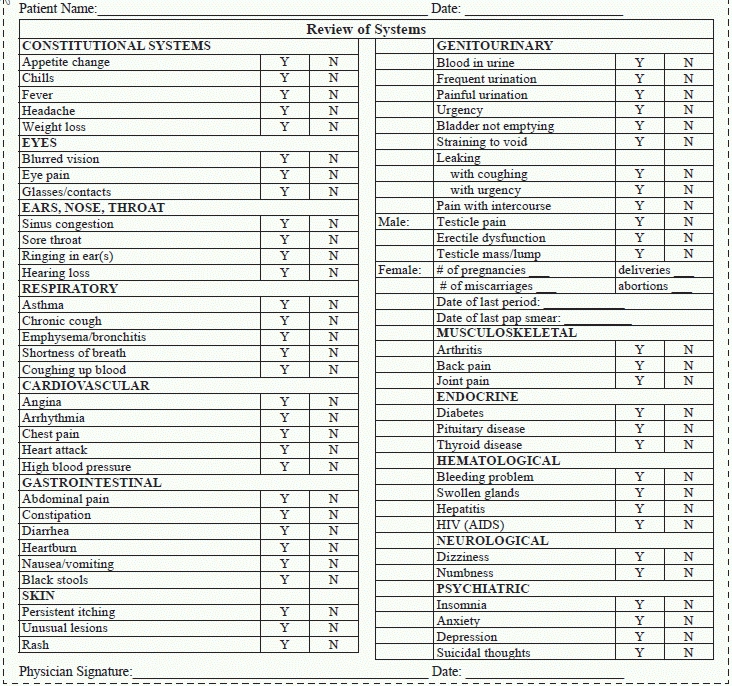
Coding a patient’s visit can be difficult when the beneficiary can’t share his history (See page 314), but even when he can, you’re still faced with other documentation issues that can trip you up. For many providers, problems can arise when the review of systems (ROS) is sparse because patients don’t report positive responses to the listed elements. However, you can still code this section if your provider remembers to document pertinent negative responses.
Background: The third element for the historical portion of an E/M service, after the chief complaint (CC) and the history of the present illness (HPI), is the ROS. This portion of the E/M service trips up many coders since they often select a lower code simply because the provider used the statement “all systems negative.”
An easy way to help your providers accurately document the E/M components you need to choose a code is to create a template they can follow. Use the following in your practice to ensure that the providers share even the negative pertinent responses to patient narratives.

.jpg)

