
Keep in mind that discharges and subsequent hospital visits cannot fall on the same day.
Have you ever wondered how your claims stack up against your peers? Comparative Billing Reports, also known as benchmarking, highlight Medicare claims trends in the industry, focusing on a particular service and specialty. Whether your claims fall within the norm or are way off the mark, this useful tool can help your practice rectify billing issues.
Part B MAC Palmetto GBA published a Comparative Billing Report (CBR) in October to highlight the trends and benchmarks that the payer has seen when Medicare providers who practice internal medicine (specialty 11) submitted claims for subsequent hospital care. Palmetto initiated the analysis “because subsequent hospital care is an area that is vulnerable to fraud, waste, and abuse,” the CBR report said in its “Frequently Asked Questions” section. “According to the Medicare Fee-For-Service 2014 Improper Payments Report, the improper payment rate for subsequent hospital visits was 20.7 percent, accounting for 2.4 percent of the overall Medicare FFS improper payment rate. The projected improper payment amount during the 2014 report period was $1.2 billion.”
Background: The feds use CBRs as a tool to offer insight into billing and coding trends across different specialties and healthcare settings. CMS partners with its contractor eGlobalTech to produce the reports, which you can find at www.cbrinfo.net. You can use the data from CBRs to see where you stand when it comes to the frequency of billing certain services, codes, or modifiers.
Take a Look at the CBR Specifics
The CBR research focused on subsequent hospital care and the claims of about 7,700 Medicare providers specializing in internal medicine. The sample was extracted on Sept. 7, 2016, and covered services administered between Jan. 1, 2015, to Dec. 31, 2015. The subjects were chosen due to their unusual billing patterns over that period of time for the following E/M codes:
99231 (Subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least 2 of these 3 key components: a problem focused interval history; a problem focused examination medical decision making that is straightforward or of low complexity ...)
99232 (… an expanded problem focused interval history; an expanded problem focused examination; medical decision making of moderate complexity…)
99233 (... a detailed interval history; a detailed examination; and medical decision-making of high complexity ...)
What auditors found: The following were the top issues that auditors discovered among the internists’ claims that caused them to be in error, said Tamara Canipe, RN, clinical quality management coordinator with Palmetto GBA, during a webinar explaining the CBR’s findings:
What the CBR revealed: Billing under the highest code, 99233, contributed to the significant error rate, said Canipe. The study highlights the need for concise notes that outline the higher quality of care. MACs are looking for E/M visit documentation with a clear focus on the medical decision making (MDM), which outlines the complexity of the service and is key in the code level choice.
She also mentioned that Palmetto GBA Railroad Medicare was doing a “widespread review” of CPT® code 99232, and the study showed that the “overall Charge Denial Rate (CDR) for the third quarter of 2016 for 99232 was 47.5 percent.”
Tip: The volume of documentation does not necessarily mean that you should bill under a higher code, Canipe reminds. “Often a lower code will work and should be used instead,” she added.
Consider These Averages
The benchmarking details allow for four possible outcomes: your billing results are significantly higher than your peers, higher than your peers, equal to your peers, and/or your results are inconclusive due to the lack of sufficient individual data, explained Cheryl Bolchoz, a Palmetto GBA statistical analyst, during the webinar.
Among the reviewed claims, Palmetto found that internists nationally averaged 27.54 minutes per visit using code 99233, despite the complex nature of the code. Other auxiliary CBR data showed that the providers discharged patients within one day of a 99233 subsequent hospital visit at around 4 percent nationally. Interestingly, 32 percent of all subsequent hospital visits were coded as 99233 across the nation.
Remember: A subsequent hospital visit and hospital discharge cannot be billed on the same day, reminded Canipe. For example, if you see the patient on the day of the discharge, choose the most appropriate code that represents the amount of floor/unit time you spend with the patient. Your options are 99238 (Hospital discharge day management; 30 minutes or less) for quick and easy discharges while 99239 (... more than 30 minutes) is used for longer goodbyes.
Check Your Numbers
The practices that Palmetto reviewed as part of the CBR received personalized reports indicating whether they billed CPT® code 99233 more or less frequently than other internists in their states.
But if you weren’t part of the sample, that doesn’t mean you’ll never know where you stand.
If you’d like to compare your usage to the average, run a calculation of your frequency of 99233 and average minutes per visit, then check out Palmetto’s results to find out where you stand in relation to the other internal medicine providers in your state.
Here is a look at the states with the highest percentages of total services billed as CPT® Code 99233 for subsequent hospital care:
Highest State Percentages of Total Services Billed as CPT® Code 99233 for Subsequent Hospital Care
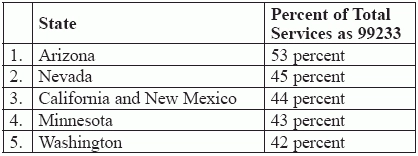
*Data from CBR 201615 by Palmetto GBA CBR and eGlobalTech: http://www.cbrinfo.net/cbr201615-statistical-debriefing.
Here’s how: “Most practice management systems should be able to generate frequency of usage of different CPT® codes,” says Vinod Gidwani, founder of Currence Physician Solutions in Skokie, Ill. “These reports may be subtitled CPT® code productivity by doctor, facility, etc.”
Once you run your reports, use the data that you glean from them to plug numbers into the average benchmarking calculations, and you’re on your way to creating a system-wide benchmarking program for your internal medicine practice.
Don’t panic: If your percentage of specific code usage is higher than the average, it doesn’t necessarily mean you’re billing incorrectly — but you should take a look at your documentation to ensure that it meets requirements. “Billing differently from your peers does not mean you are an outlier or that your claims are wrong,” Canipe said during the webinar. “Claims differ due to geographic location and patient acuity levels,” she explains. “Subspecialties can also skewer results and might not be evident in your claims data.”
Resource: To read more about the CBR for subsequent hospital care, visit www.cbrinfo.net/cbr201615.
