Here’s how to stop letting the similar names muddy your coding.
The terms “epidural steroid injection” (ESI) and “translaminar or interlaminar injection” might be interchanged sometimes, but don’t let the names confuse you. Neither is the same as a transforaminal ESI, so keep reading to learn the difference.
Get to Know Your ESI Code Options
CPT® includes four codes for epidural steroid injections. The first two represent a single-shot epidural injection:
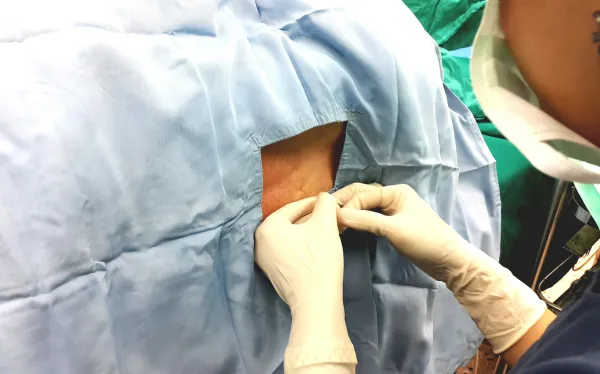
During the procedure, the provider uses fluoroscopy to guide needle placement between the vertebral lamina near the spinous process and confirm that the tip of the needle reaches the epidural/subarachnoid space before he or she injects the medication. He uses the subarachnoid route when trying to inject the medication directly into the cerebral spinal fluid. An epidural injection deposits the drug(s) outside the dura.
Your provider administers the ESI to the cervical or thoracic spine for patients who have pain in the arms, neck, chest, or upper back area. A lumbar or caudal epidural injection can help treat pain in the legs and/or lower back/buttock(s) area.
The other two ESI codes are for administration by continuous infusion or intermittent bolus via a catheter left in place for a prolonged period, i.e., more than a single calendar day:
For this administration, the provider threads a catheter through the spinal needle into the epidural space and then removes the needle. A continuous infusion can last for several hours or days. Occasionally, the provider might need to give three or more injections through the indwelling catheter over a period of hours/days and may use different drugs.
Pay attention: All four ESI codes include the injection of contrast material. If your provider uses fluoroscopic guidance during the procedure, you can bill the fluoroscopy separately with 77003 (Fluoroscopic guidance and localization of needle or catheter tip for spine or paraspinous diagnostic or therapeutic injection procedures [epidural or subarachnoid]). Append modifier 26 (Professional component) to indicate your provider’s role in administering the injection if he performs the procedure in a facility (you won’t append a modifier to 77003 if he administers the injection in his office).
Also: Medicare’s stance on these procedures will change in 2015, when CMS won’t pay separately for 62310-62319 with fluoroscopic guidance. “This may not be the case for all payers, though, and certainly won’t be the stance of CPT®,” says Marvel J. Hammer, RN, CPC, CCS-P, PCS, ACS-PM, CHCO, of MJH Consulting in Denver, Co.
Look at the Transforaminal Epidural Difference
A transforaminal ESI is more difficult to perform because of how close the nerve root your provider targets is to the spinal cord and blood vessels. Providers use fluoroscopy during transforaminal ESIs for precise anatomic localization and to avoid injecting into and/or injuring the vertebral artery.
You have four CPT® code choices for transforaminal epidural injections, based on the spinal level treated and the number of injections administered:
The code descriptors were revised in 2011 to include fluoroscopic guidance. Therefore, you should not bill image guidance separately with 77003.
Good note: These codes represent unilateral procedures. If your provider administers bilateral injections, indicate this on the claim by appending the RT (Right side)/LT (Left side) modifiers or modifier 50 (Bilateral procedure) to the injection code, depending on what the payer guidelines state.
Stay Alert for Bundling Issues
Correct Coding Initiative (CCI) edits bundle some of these injection procedures together so you cannot bill them when performed at the same spinal area when reporting to Medicare or other payers that follow CCI.
Example: The physician administers a L4-L5 ESI (62311) and a L5 transforaminal ESI (64483) at L4-L5. CCI bundles the transforaminal epidural as a mutually exclusive procedure so you can only bill 62311.
