Spot Shot Site Before Coding Morton's Neuroma Injection
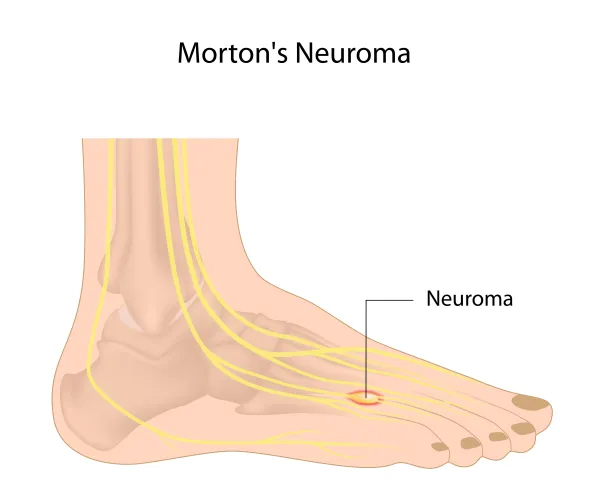
Question: I have a puzzling claim in front of me. Notes indicate that the provider performed a steroid injection on a patient with "Morton's neuroma." I reported 64479 and received a denial. What did I do wrong? Oregon Subscriber Answer: You'll need to confer with the provider, but you likely chose the wrong injection code. When you re-submit the claim, you might also want to consider appending the proper ICD-10 diagnosis code. Do this: First, go back and check with the provider about the injection site and its purpose. If the provider says that the injection site is in the foot area, especially between the toes, then you'll likely choose 64455 (Injection[s], anesthetic agent and/or steroid, plantar common digital nerve[s] [eg, Morton's neuroma]) for the injection. According to mortonsneuroma.com, "Morton's neuroma (also known as Morton's metatarsalgia, Morton's neuralgia, plantar neuroma or intermetatarsal neuroma) is a thickening of the nerve that supplies sensation to the area between the toes." The website goes on to explain that symptoms of the condition typically occur on one side of the foot, and can include: If the encounter notes reflect any of the above conditions, it's a good bet that you should code the injection with 64455. The code you chose, 64479 (Injection[s], anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance [fluoroscopy or CT]; cervical or thoracic, single level), is for cervical/thoracic steroid injections. ICD-10 reminder: If you are sure that the provider has a diagnosable case of Morton's neuralgia on this claim, you should append the appropriate diagnosis code to 64455; for this condition, you'd choose G57.6 (Lesion of plantar nerve...) to represent the neuralgia.