Use 26 to Separate Codes, Affirm Correct Coding

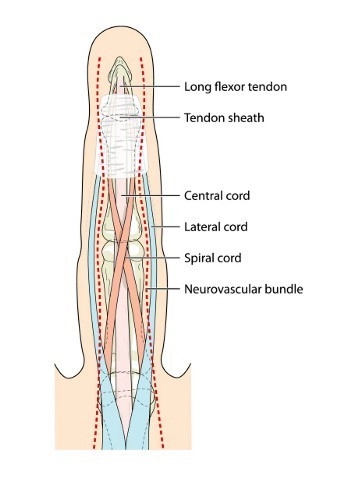
Connect with TC provider on 26 claims to compare notes. Coders at PM practices will likely do the bulk of their coding for services the provider furnishes in the office, with the practice’s own equipment. What happens, however, when the provider performs services using someone else’s equipment and/or facility? That’s when you’ll need help from modifier 26 (Professional component). So if you want to know the best and most effective ways to deploy the modifier for maximum efficiency, read on for our experts’ feedback. Could you explain when a provider will need to use modifier 26? “Modifier 26 is utilized with CPT® code(s) that are a combination of professional and technical components. This is also known as “global” procedure(s) / service(s). This modifier indicates that the physician (professional component) is the only part of the service / procedure being reported,” explains Yvonne Dillon, CPC, CEDC, coding consultant in Indianapolis, Indiana. According to Kelly Dennis, CANPC, CHCA, CPC, CPC-I, owner of Perfect Office Solutions in Leesburg, Florida, some procedures are a combination of both a physician component and a technical component. “Using modifier 26 identifies the physician’s component. When a 26 modifier is reported, it reduces payment to just the physicians work, not the cost of the equipment,” continues Dennis. Obviously, you should be on the lookout for modifier 26 scenarios anytime a provider is performing services off-site. According to Dillon, you’ll use the modifier most often for providers “who perform the professional component only of the procedures/services provided within facility-owned locations.” The locations where modifier 26 sees the most work include, but are not limited to: Could you give me a few examples of encounters in which you’d have to append modifier 26? A common scenario in which PM coders might need modifier 26 involves diagnostic studies or tests, when the equipment is owned by a separate entity. For example, a physician performed placement of central venous access device with ultrasound guidance in a hospital setting. You would report +76937 (Ultrasound guidance for vascular access requiring ultrasound evaluation of potential access sites, documentation of selected vessel patency, concurrent realtime ultrasound visualization of vascular needle entry, with permanent recording and reporting (List separately in addition to code for primary procedure)) with modifier 26 appended. The hospital, or whichever entity owns the equipment, would report +76937 with modifier TC (Technical component) appended to show that it is only billing for the technical portion of the code. Here’s another example, courtesy of Suzan Hauptman, MPM, CPC, CEMC, CEDC, director, compliance audit, Cancer Treatment Centers of America. The PM physician treats a new patient at the local hospital for an evaluation and management (E/M) visit. After performing history and exam, along with medical decision-making (MDM), the physician decides to send the patient down the hall for a single-view spine X-ray. After the X-ray, the physician writes and interprets a report. For this encounter, you’d report 72020 (Radiologic examination, spine, single view, specify level) for the X-rays with modifier 26 appended. Explanation: “The physician doesn’t own the equipment down the hall as it is part of the hospital, so he can’t bill for the technical component,” explains Hauptman. Line Up With TC Provider to Ensure Proper Coding Obviously, it behooves you to know what the provider who furnishes the equipment is coding when you report a modifier 26 claim; if your code doesn’t match the code the other provider files, there will be confusion and, possibly, a denial. In order to make sure your coding lines up with the other provider’s, you should check with the other provider before filing the claim to make sure you are on the same page. “It is always best practice to make sure both providers are billing appropriately,” says Dillon. “This can be done by getting a copy of what the other provider has coded for the procedure/service provided.” If there is a discrepancy in coding, you should contact the other payer and discuss the situation before filing the claim. In a nutshell: Hauptman says the easiest way to make sure you use modifier 26 correctly is to: a. “Understand what is included in the description of the code — some codes are for only the professional component and you wouldn’t need the 26 modifier. Trouble Could Lie Ahead for Modifier Neglecters If you don’t append modifier 26 to the claim when it is required, you’re walking a dangerous line. If the claim goes through, the practice will get paid for something it didn’t provide — the technical component of the code. “It is important to make sure you recoup only the money for the professional component. The OIG [Office of Inspector General] watches the professional services, and the -26 modifier, very carefully. Make sure you understand all of these requirements,” advises Hauptman.
b. “Understand exactly what your physician did and read the documentation associated with the service.
c. “Know what equipment is owned by your practice and what is owned by the various facilities where your doctor sees patients.”